“’Is that blood?’ I asked my mom at 10 years old, showing her the underwear I had taken off. She confirmed I was having my first period. Everything was textbook until it wasn’t. I paid more attention to my cycles around 16 years old. I would skip months or several months at once. I just knew something was wrong, yet convincing medical professionals of this proved to be the ultimate difficulty. At 18, I became very concerned.
I saw a gynecologist who did not take my concerns seriously, and later, I found out they didn’t even run proper tests. ‘Can you please check my hormone levels? I know something is wrong,’ I desperately begged. It was over 90 days since my last period. I was told they would get better the older I become, but that simply was not true—in fact, it became worse the older I got. I had an appendectomy but somehow the general surgeon made it a point to list out in the report that nothing was wrong with my ovaries or fallopian tubes.

My concerns, after a visit to another gynecologist, were once again ignored. ‘I’m worried about my future fertility since my periods are so irregular and painful.’ She assured me that since I wasn’t actively trying to get pregnant, I had nothing to worry about and said there aren’t tests for fertility. She told me to use a heating pad on my stomach and back along with extra doses of Tylenol. ‘Do they make full-body heating pads, and who needs a liver anyway?’ I thought. The doctor continued to dismiss my worries, ‘It’s not like you have polycystic ovarian syndrome or anything, you’re not overweight or hairy.’
Apparently, since I was not trying to have a baby, my own health simply did not matter. She was wrong though. She was so wrong. My health did matter, and I was determined to find someone to listen to me. I took it upon myself to schedule an appointment with an endocrinologist since I felt like gynecologists were just not taking me seriously. I brought in a list of all of my symptoms and the exact dates of my seven periods that whole year. My acne was worse than as a teenager, prompting me to take antibiotics from the dermatologist for 6 months. He listened to me and took my concerns seriously. I did some blood work and got a call about a week later. ‘Your hormone levels are consistent with polycystic ovarian syndrome.’ I thanked him through sobs. ‘Finally, someone listened to me,’ I thought. I knew for years what other doctors were attempting to brush off.
My periods continued to get worse. I had to drop out of college because I couldn’t manage constant pain, college, and working. As time passed, the pain from my monthly cycles became a daily occurrence. I would pass out and throw up from the pain at times. My pelvis would ache 24/7 into my back and legs. I took Epsom salt baths for temporary relief. Sleep was the only escape, yet the second I woke up, I instantly felt pain. I was pretty depressed dealing with chronic pain and even felt suicidal at times. I wasn’t sure how I was supposed to live like this. I wasn’t even living, merely surviving, and that became problematic to me. My gynecologist prescribed me Tylenol with codeine and eventually Tramadol. I asked myself how any of this was normal.
By March 2015, I was being wheeled into the recovery room hysterically crying after being told I had endometriosis. ‘But I already have PCOS.’ Until a nurse tried to calm me down. In that moment, I sobbed for everything I thought my life would be, and for everything I desperately wanted it to be. I felt so broken. I was angry for a long time. I wanted nothing more in this life than to be a mother. I talked to that same gynecologist that had performed my first laparoscopic surgery and asked about my future fertility at my post-operative appointment.
‘With having polycystic ovarian syndrome and endometriosis, you should try to have a family by 28 years old, but do not settle…wait for the right guy.’ ‘Well, of course,’ I thought. In the end, he had given me six years to somehow get my life together. ‘Maybe you can just take a pill to induce ovulation or maybe you’ll need more intervention, but right now we do not know,’ the doctor told me. I was told I had endometriosis on both of my uterosacral ligaments and that my left ovary and fallopian tube were adhered together. I knew having polycystic ovarian syndrome and endometriosis could potentially make things more difficult. I felt like I had done something to my body for it to fail me. May 2018 came around and I went through another laparoscopic surgery since my pain came back. My bowel was covered in adhesions and attached to my ligament, pulling it in one direction. I had a small speck in the middle of my bladder. My left fallopian tube was attached to the left ovary again. The right uterosacral had some lesions. Other lesions were found on the left uterosacral ligament. I had a pocket behind the uterosacral ligament. Lastly, I had a procedure to look at my bladder. With that, I was also diagnosed with interstitial cystitis. I completed physical therapy for pelvic floor dysfunction as well.
Society associates a woman’s worth with their ability to have a child, so how could I possibly fit in here? I focused on myself and had given up on the dreams of me having my own family, as dramatic as that sounds in one’s 20s. I finished an associate’s degree, a bachelor’s degree, and even a master’s. I even met a man that I could see myself with—he already had a child from a previous marriage, but I spent time thinking maybe I had finally met someone to spend my life with and even thought about having my own family again.

My husband and I began our fertility journey in March 2021 before we got married. I wanted to get our preliminary testing done because I knew from reading other people’s stories that it could take some time to complete and move forward with a plan. I had 11 vials of blood drawn along with another procedure while my husband had maybe two drawn. My hysterosalpingogram, also known as the tube test, came back clear which was great considering my previous surgeries. After a month the testing was finally done.

We opted to do genetic carrier testing and waited for results. Our clinic had us watch some videos explaining fertility and genetic testing. Of course, we laughed through the whole genetic testing video thinking, ‘We took science class already, this is so pointless.’ My husband’s testing came back perfect aside from 2% morphology which was of no concern to our reproductive endocrinologist. Overall, testing revealed polycystic ovarian syndrome was the main concern. Our reproductive endocrinologist had given us a couple of options. We could move forward with timed intercourse where I would take a pill to induce ovulation or intrauterine insemination where they would directly place sperm into the vagina at the right time. We were so excited! ‘Maybe I can just take a pill,’ I thought. We met with our genetic counselor to review our results before proceeding.

‘You were each tested for 283 genetic diseases. These conditions focus on infant and childhood-onset conditions so things that cause birth defects, intellectual disabilities, or some sort of severe medical issue in babies and children.’ The genetic counselor continued on, ‘We have two copies of every gene, and if you’re a carrier of something it means that one copy of the gene is normal and the other copy has a mutation and it’s not working. But because we have a backup copy of every gene being a carrier doesn’t cause you to develop symptoms of that disease or generally doesn’t cause you to become sick in any way. It’s only when two parents are carriers of the same genetic condition that there’s a one in four risk for each child or each pregnancy to be affected by that condition.’

‘We already heard this in the video our clinic had us watch.’ I thought she was just reviewing information until she continued talking. ‘So you actually are both coming back as carriers of the same condition…congenital disorder of glycosylation type Ia.’ My mind went blank. ‘How common is this really?’ I thought. Only 5% of couples carry the same genetic mutation. The genetic counselor continued ‘It’s a spectrum of severity, so some patients with this disease have a more-mild presentation and some more severe. Unfortunately, you both carry the same mutation, and it is one of the more severe mutations.’ I immediately cried. Nobody wants to hear any possible child has a one in four risk of developing a disease. ‘This is not how this was supposed to go,’ I thought. ‘It’s been noted in the literature patients who carry the mutation that you carry in combination with a different or more mild mutation there are reports of people living with that condition. But there aren’t any reports of people living with two of the mutation that the two of you carry. So the assumption in the scientific community is that because it’s such a severe mutation it is fatal either during embryonic or fetal development or very quickly after birth.’
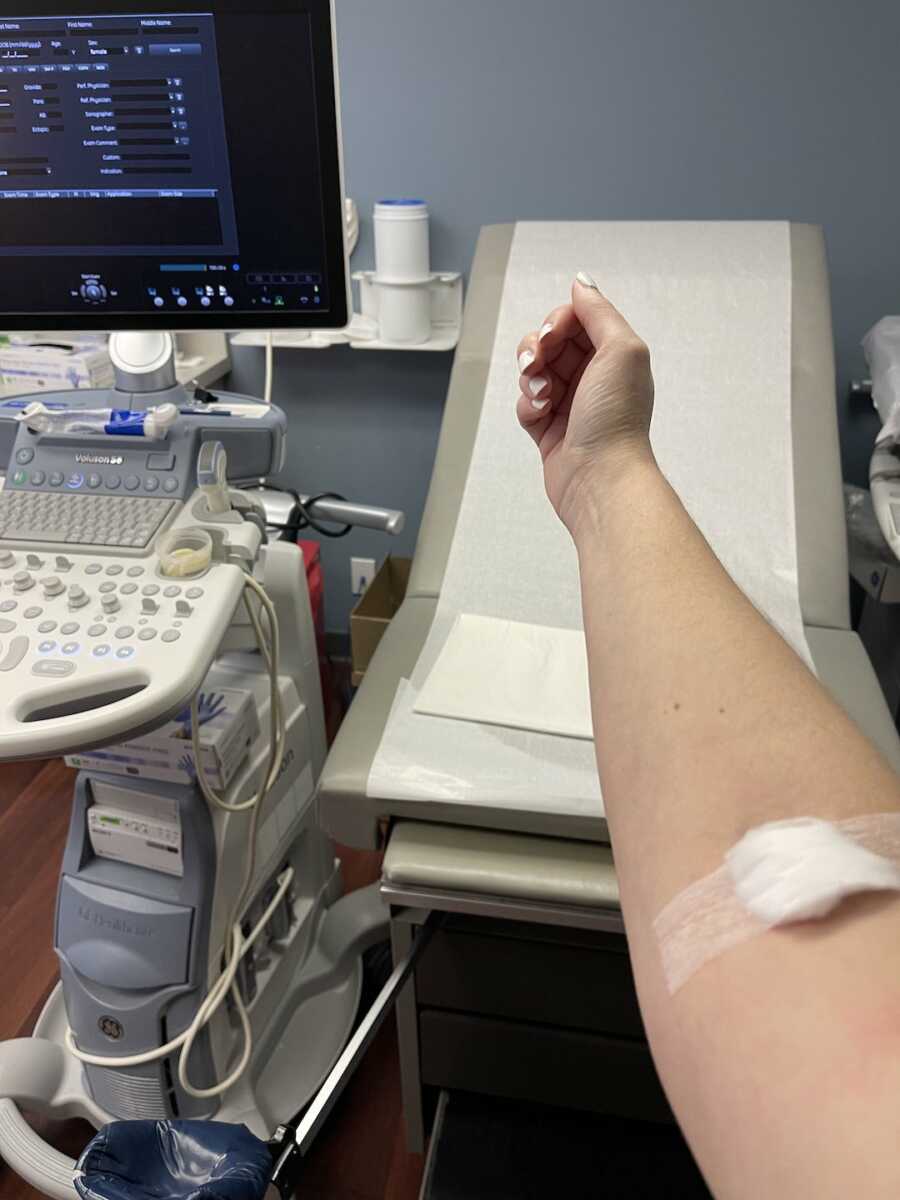
We went through 2 rounds of IVF. The shots became easier as time went on. I had bruises on my arms from blood draws at my clinic checking my hormone levels and even developed bruises on my stomach. I had multiple ultrasounds during each round to check on follicle growth. The things I was willing to do for a chance at a child paled in comparison to my desire to be a mother. ‘If we have 3 genetically healthy embryos, the chance of getting at least one baby is 95%.’ Our reproductive endocrinologist has been so informative during this process. One transfer would yield a 65% success rate, two would yield an 80% success rate, and three would yield a 95% success rate. For one baby. We knew we wanted two more children so statistically, we would need four to six healthy embryos to give us a good chance at that. Our first round produced 18 eggs, 15 were mature and injected with a single sperm, 13 were fertilized, nine made it at least five days in the petri dish and became a blastocyst. We opted to do preimplantation genetic testing which checked for 46 chromosomes as well as genetic testing to test embryos for the genetic mutation. Four out of nine were chromosomally abnormal. Three out of five that were chromosomally normal had congenital disorder of glycosylation. We got two carrier embryos we could freeze for the future. Of course, we were happy to get these two.

We were also pretty naïve going into it and hoped that one round would give us the results we were looking for. Our second round of IVF produced 34 eggs, 24 were mature and injected with a single sperm, 15 were fertilized, and 6 made it at least five days in the petri dish and became a blastocyst. We thought we would not have anything to freeze, but every cycle can be so different. One embryo was chromosomally abnormal and none had congenital disorder of glycosylation. We had four embryos to freeze that were carriers with one of them being a non-carrier. Another one of the carrier embryos had a mixture of normal and abnormal cells having more normal cells that we could keep as a low priority for the future. Altogether after two rounds of IVF, we had seven embryos that could potentially become our child(ren). We began to feel hopeful again and felt like we had a good chance at making our dreams a reality! Our infertility journey is still ongoing but we know because of our doctor and team that we have a good chance at a healthy child.
There is so much stigma, shame, and lack of education surrounding infertility. Fertility treatment is never guaranteed yet couples turn to it each year just for a chance to make their dreams come true. Luckily, our families have been nothing but supportive. Our parents even used their DNA to help make a genetic probe to test our embryos for the genetic condition. But as a society, there is a lot that people do not understand regarding fertility treatment. It is so difficult. Physically, mentally, and emotionally. It takes a toll on every aspect of someone’s life. It becomes the main focus of life for a while. I have been through a lot in life, yet infertility has been a whole new kind of hell. Questioning, wondering, and hoping that it will finally work for us.
I know not everyone will relate to this story, but everyone can take away some main points from my story. You know your body better than anyone else. You need to be your own advocate. Do not stop until someone will listen to you. You deserve to be heard—not because you’re trying to have a child but because you deserve to be informed on your body and your own health. You are worthy of that knowledge!”
This story was submitted to Love What Matters by Michelle McMahon from Saint Louis, Missouri. You can follow her journey on Instagram and YouTube. Submit your own story here. Be sure to subscribe to our free email newsletter for our best stories, and YouTube for our best videos.
Read more touching stories like this:
Provide hope for someone struggling. SHARE this story on Facebook with family and friends.



