Disclaimer: This story includes images of child loss that may be triggering to some.
“‘I’m sorry, but the severity of the hygroma leads me to believe the baby will not make it.’ ‘Not fit for life,’ is what they told us. ‘You won’t make it past three months.’ Hearing these words come out of the specialist’s mouth was the last thing we expected to hear. We were 14-and-half-weeks pregnant with our second child and I’m pretty sure, at this point, my faith in the universe was diminishing. Becoming mothers has taken my wife, Lisa, and I down the road less traveled. Over the past 3 years, there have been nine IUI attempts, four miscarriages, one amazing little girl rocking an extra chromosome, one round of IUI injectable, one round of IVF, and one vanishing twin. Now this, our little babes was given a terminal, not fit for life diagnosis.
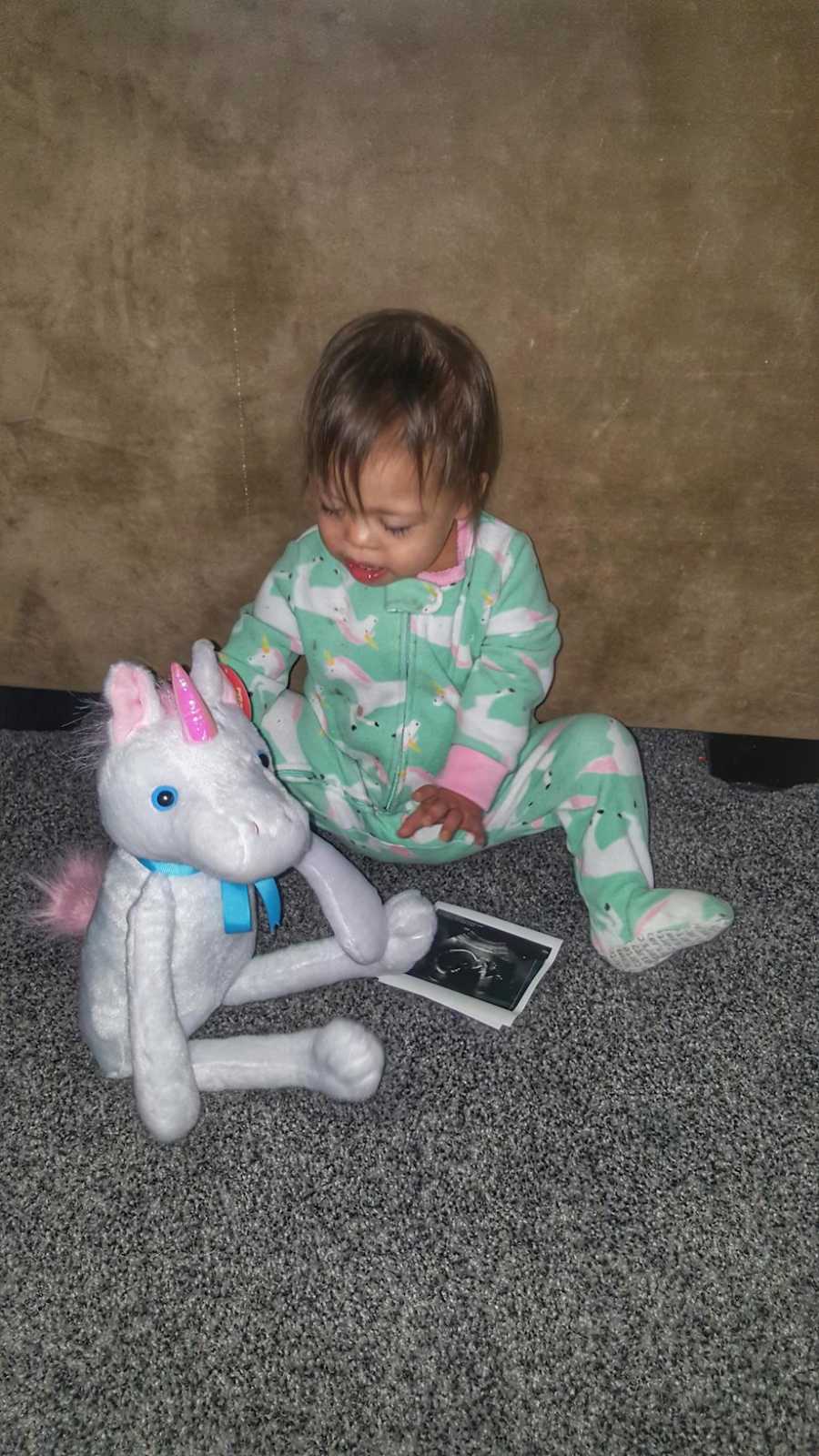
Getting pregnant and being released from Mid-Iowa was as far as I had ever gotten in pregnancy. All of my miscarriages and failed attempts had all happened in the first trimester. So when I got to make the first appointment with our OB, I was thrilled. I mean, this was the furthest I had ever made it. We went to our appointment, had our ultrasound, and waited for the doctor to come in. ‘The ultrasound showed some areas of concern. This area back here is the nuchal fold…’ I looked at Lisa. Talk about the biggest exhale and deja vu. You see, it sounded exactly like the start of a conversation we had when Lisa was pregnant with our daughter, Addi, who has Down syndrome. I kindly interrupted the doctor and said, We have been down this road. We will set up an appointment with the specialist.’ They took blood for the NIPT test, which two weeks later, came back negative for any chromosomal abnormality. So, we figured going to the specialist was going to be routine. Boy, were we wrong.
Of course, we didn’t get to see the specialist we normally saw and after our ‘not fit for life’ diagnosis, we wanted to reschedule with our normal one. The time waiting for that appointment took forever, and every thought crosses your mind. ‘Was the NIPT test wrong? Did I do something wrong? Could this have been discovered had we done preimplantation testing?’ The list goes on.
At 19 weeks, we got to go in and see our regular specialist. We had a growth and anatomy scan first and got to see our little baby on the screen. The sonographer knew us from our first pregnancy and knew there were already complications with this pregnancy. She did an amazing job telling us all the good things. For me, at this point, it’s the most apprehensive feeling holding your breath and waiting till you hear a heartbeat. So every time I did hear the heartbeat, it was like a breath of fresh air. After you have one high-risk pregnancy, you pick up on things or learn to ask a lot of questions. ‘Can you see all four chambers of the heart? Is the midline of the brain good? Is there fluid anywhere there shouldn’t be?’ When the sonographer starts typing things out on the screen, you remember what they are to look up later.

After the ultrasound, we went into the consultation room and waited for what seemed like forever. We googled what the sonographer had typed out on the screen and learned that babes had a two-vessel umbilical cord. The nurse even came in at one point and said the doctor was going to see one more person first. After about an hour or so of waiting, our doctor came in, and the look on her face was one you just never want to see. She apologized for making us wait but wanted to check everyone out so she could spend as much time with us as needed. She then went on to tell us she hated coming in to tell us what she had to. Everything was much worse than she was led to believe. There were a variety of issues going on with babes. There was a diaphragmatic hernia, in which all of the bowels had moved up into the chest cavity. She couldn’t see a stomach anywhere. There was only one kidney, the left arm had seemed to not be developing, and I had little to no amniotic fluid. Que a whole lot of tears. Taking in all this information is like having the wind knocked out of you from taking a punch to the gut. You don’t even know how to respond or what to say.
One of the reasons we love our specialist is because she explains everything and keeps it real. But she does so in a very compassionate way. She explained, had it just been the hernia, we could have gone to a hospital in Pennsylvania that does in utero surgeries, but with the other concerns, they wouldn’t do it. She said very carefully she knew from previous experience with our daughter, Addi, that termination was not something we ever wanted to do, but she did put it on the table. She then asked what we wanted or what our goals were. We could come back and see her as often as we wanted or never again, if we wanted to just let nature take its course. She did say that she believed we would have a stillbirth but also wanted us to get connected with the perinatal hospice team. We did go to Iowa City to get a second opinion but the outcome was the same.
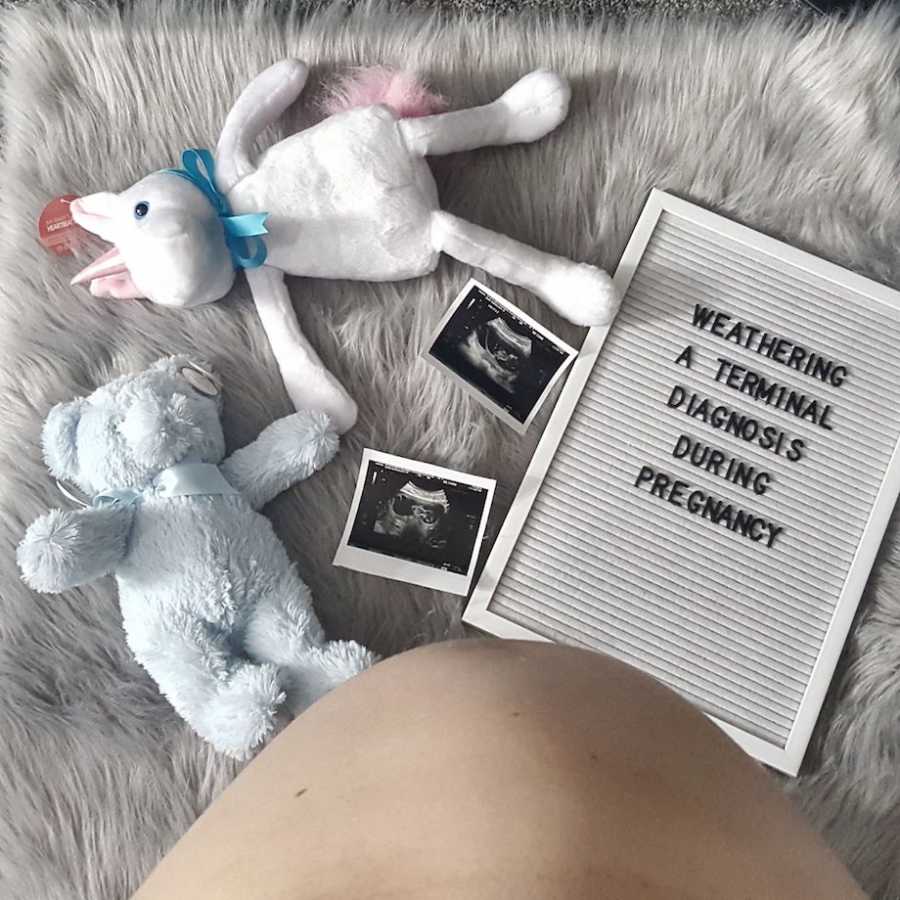
What do you do? Well, for us there were a lot of tears, a lot of hopes for miracles, and a lot of questioning life. We knew termination was not something we wanted to do, so instead, we decided to celebrate. We decided, however long we got to have our babes, he was going to be loved, he was going to experience life, and he was going to share his story. Over the next few months, we met with the neonatal surgical team, whose recommendation was comfort care but when and if I got closer to live birth, we could meet again to discuss what medical intervention looked like. We had our biweekly check-ins with the OB and specialist, who were amazed by how much he was growing, how much he was developing, and at one point, finally explained if we were going to have a stillbirth due to the complications, it would have happened already and we would indeed probably make it to a live birth.

Meanwhile, we announced to our friends and family what was going on, did a gender reveal telling everyone we were having a little boy, went to a bunch of concerts, took maternity pictures, ran lots of races and even a triathlon (indoor), had some amazing adventures, and celebrated his 200-day birthday. I remember writing about hope.
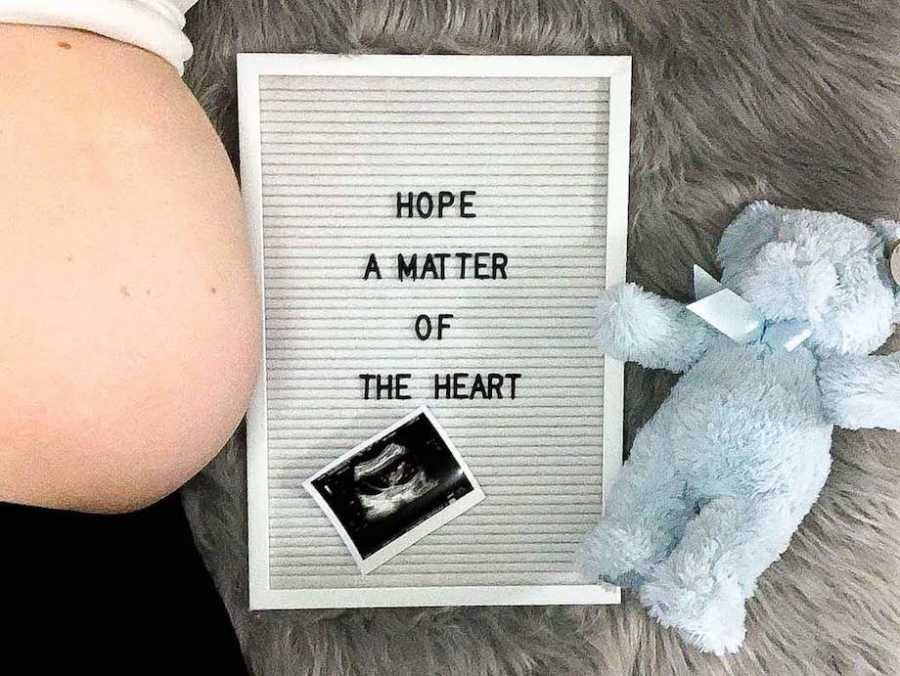
Hope–a matter of the heart. To me, hope isn’t necessarily a tangible thing. It’s a matter of the heart. It’s not about luck, percentages, or prognosis. It’s not about numbers, quality of life, outcomes, or opportunities. It’s a feeling, it’s a thought. It’s that thing or idea we think about and we hope will happen. Hope can give us courage. Hope can help us persist in the face of adversity or aid in getting through our current journey. For me, hope is flexible. It changes with the situation and sometimes, it changes with each doctor’s appointment. Right now, I hope for time. Time to get to live birth, time to meet our little man, and as much time as we can have with him.
The flip side to all of this is coming to terms with the reality of the situation and while we were making a birth and journey plan for live birth, we also had to make a birth and journey plan for the alternative. The idea of planning a funeral for your child is the absolute worst, most devastating, soul-sucking feeling there is, yet it was something we had to do.
On the evening of June 12th, we had gotten home from another busy day of just life. I hadn’t been feeling the best and went to lay down, figuring I was just worn out. I knew we had a specialist appointment the next morning and then an appointment with the neonatal surgical team in the afternoon. At this point, we were 35 weeks pregnant. However, I ended up getting sick for the next few hours and started having the worst back spasms. Finally, at 2 a.m., I woke Lisa up and said, ‘We have to go!’ We got to the hospital and they just figured I was dehydrated and gave me two bags of fluid, did an exam, and sent me home. I went home, tried to lay down but these back spasms were not going away and actually getting worse.
We got to our specialist appointment at 9 a.m., did the growth and anatomy scan, and all I remember is his heartbeat was strong. We went into the exam room and as soon as the nurse came in, she said, ‘Are you in labor?’
She went and got the doctor. When she came in, she said, ‘Are you trying to have a baby in my exam room? Get over to the hospital.’ We went across the parking lot, were admitted–again–and when I got hooked up to the machine at 10:49, I was already dilated to a three. The doctor came in and was trying to talk to me about a bunch of different things but all I could keep thinking was, ‘It’s too early. We were supposed to meet with the medical team at 2 p.m. This wasn’t supposed to happen.’

Before I knew it, the doctor checked me again and said, ‘Patty, I can feel him, we have to go.’ There was no time to talk, make decisions, or even get an epidural. At 12:32, Hudson Drake was born, weighing 3 pounds, 15 ounces, and 14.25 inches.


We were able to spend about 35 minutes with Hudson before the doctor called his passing. In hindsight, I am thankful there was no epidural or any anesthesia because I wanted to be fully present for every minute I could have with our son. All I could do was tell him, ‘We love you, thank you for teaching me so much, I am so sorry.’ That is when he had his last heartbeat while laying on my chest.
We were taken back to our room, a room I will never forget. We stayed at the hospital for 2 days, in which Hudson did not leave our side. We tried to do all the things; gave him his bath, took handprints, footprints, read stories, and sang songs. A dear friend came and took pictures. We even had his baptism and last rights given all at the same time. Pretty sure I didn’t sleep the entire time we were at the hospital because, at the time, it seemed like a waste. I didn’t want to waste any moment I could have with him. It was hard not to notice his body changing, the color leaving, his skin hardening, and getting so cold. I often wonder if I made the right decision keeping him with me for so long–but I know I did. Then the time came to hand him over. The nurse kept telling me to take as much time as I needed and I finally had to tell her, ‘If you keep telling me that, I will never leave.’


The next week was filled with planning the funeral, meeting with people, and barely being able to do much. If it wasn’t for certain people stepping up and taking care of everything, I’m not sure they would have gotten done. There was a lot of silence but in a good way. We would go for walks and I would see things I never noticed, even though I had walked the area a million times. Butterflies and cardinals often come to visit and I know it’s Hudson saying hi.
I truly believe the quality of life has nothing to do with its length and Hudson’s life–however short it may have been–was lived to the fullest. I know, looking back, he made all the decisions for us. He knew we had that appointment with the neonatal surgical team the afternoon to decide between comfort care and medical intervention, and it was his way of saying, ‘I don’t want to put the burden of making that decision on you. I’ve got this.’ He also gave me the biggest gift of all: he made me a mother. He proved I can do all these things and I do not regret one decision we ever made.

Navigating this journey of child loss is a conflicting one for me. There is all the grief that comes along with it. The loss, emptiness and numbing feelings of things you will never get to experience with your child. The daily doses of tears, having to answer questions like, ‘How many kids do you have?’ But there is also the joy in his story and gratefulness that he picked me/us to be his mothers. We get to share his story. We can help others experiencing loss and grief and how his story inspires others.

As the days continue to come and we let the light in little by little, we learn to carry the tragedy of child loss a little differently. Life will never be the same, for we are forever changed but we still have the power to continue writing his story–Hudson’s story.”
From podcasts to video shows, parenting resources to happy tears – join the Love What Matters community and subscribe on YouTube.


This story was submitted to Love What Matters by Patty Sneddon-Kisting of Des Moines, Iowa. You can follow her journey on Instagram. Do you have a similar experience? We’d like to hear your important journey. Submit your own story here, and be sure to subscribe to our free email newsletter for our best stories.
Read more by Patty Sneddon-Kisting:
Read more touching stories like this:
Provide beauty and strength for others. SHARE this story on Facebook with family and friends.

