“My daughter, Rose, has a rare genetic disorder, Trisomy 18. She also has congenital heart disease. Her diagnosis is considered ‘incompatible with life.’ As a result, finding her the full medical care she needed at birth and after is a challenge. It is considered futile to offer many life-saving interventions to children with this and they are often denied care. This is the story of our journey of Rose’s life-saving medical care. A story told by me, her mother. It’s a story of broken hearts seeking repair.
‘Mrs. Willard, can you have a seat right here?’ This was the first jab that punctured my familiar bubble of pregnancy. So naive to ‘genetic disorders’ and how they derail medical care, I sat down happily and began to search for my phone to text my husband. My mom was home with our five other children and my husband busy at work. I headed to this sonogram alone. Alone in a chair at the end of a hall, I texted my husband and mom, ‘I am done, it all looks good. I saw the little heart, sac, and tiny little baby. All looks normal.’ This was the last time in Rose’s life she would be called ‘normal’ in a medical setting.
‘Mrs. Willard, can you come with me?’ A little curious why I was asked to sit in this chair by the receptionist, but not too concerned, I waited. A lady approached me. She asked if I had the ‘genetic screening‘ done. I said I had, but received no information from it and assumed it was a good sign. She nodded and said, ‘Mrs. Willard, can you follow me?’ Jab, this time I felt my heart drop. I lifted myself from the chair, and in a dizzy haze followed her back to a small room.
This was not familiar. Like arriving at the loading dock of a roller coaster, once she closed the door I was locked in my seat beginning the ride of my life. I had no choice but to hang on tightly. Clenched, sweaty hands, heart racing, breath-holding, anticipation for the big drop and loop, yet eyes clenched shut and unable to scream, I sat in anticipation. Every muscle tense and jelly in one. Leaving me staring across the desk, vulnerable and clueless for what ride I was on.
‘There are some signs showing a concern.’ I didn’t respond. I waited. I assumed this could be based on my age, a pressure for genetic testing, cystic fibrosis, or other concerns. I stayed silent and waited for the plunge down. I remember for a split second having this strong feeling. A peace, a knowing my child was ‘okay.’ I relaxed a bit. I became more curious than scared, and I began to tap one foot on the floor to remind myself to be grounded. To stop the roller coaster. To pause and be present. I listened. I heard only some of what she said. The main points were the information analyzed by sonogram showed a high risk for a chromosomal disorder. This is not Trisomy 21, AKA Down syndrome. This is worse!
She gave me a packet and told me, ‘This is not a viable pregnancy. You need to see the doctor ASAP. He can see you tomorrow. This diagnosis is not compatible with life. There is a procedure you can schedule you. Have some time, but you can’t wait too long.’

‘The doctor will tell you more tomorrow. The genetic counselor will call you.’ I left the room hot in the face, stumbled to the waiting room, and out into the hallway, the same one that just hours ago held such joy. It still did for others, but not me. What would tomorrow lead to? I felt like I didn’t belong there, amongst the happy, healthy, pregnant women. I felt like I would never be ‘normal’ ever again. I was right. I am forever changed. The next few months were filled with conversations with the specialist, geneticist, and my family and friends about Trisomy 18. And I was put in the position of a poorly trained translator in the language from specialist to specialist, then to our loved ones.
‘Why is she keeping it?’ I was already facing flat affect and dismissing my child’s worth from medical staff, but now this question was asked by a loved one. Jab, jab, stab. Ouch, it hurt. It still hurts. It further divided me from others. One more event validating what I already knew: this is not a typical child, I am not a typical mom, we will never again get to be typical. And many will ask, ‘Why?’ And I won’t answer them. I never asked myself ‘why.’ I never asked God ‘why.’ I never felt guilt or shame that my child’s chromosomes divided in a unique way. I didn’t waste time asking why. I did have a huge dominant question that filled my heart mind and soul: ‘what.’ What is this condition? What do we do about it? What resources are there for us? What am I going to do? What will this look like, what will my child look like, what will our lives be like?

‘What do you want to do?’ The genetic counselor and I had been playing phone tag. It was getting late in the day and I decided I would stop watching my phone for her call. I took a deep breath, turned on the Moana soundtrack, and delighted in my time to dance with my boys and imagine a sweet little baby girl joining our dance parties one day. ‘No one knows how far I’ll go’ were the lyrics that choked me up. I sat down and let the song crash down on me. Like waves, the lyrics inspired and taunted me. I was no longer holding my little one’s hands as they were jumping and twirling. I was sitting in a poised position, hanging on to every lyric. Like some place hope in a positive fortune cookie or search for a sign from God, the lyrics were jabbing at me. Actually poking at me. Poking through me, my bubble was almost deflated at this point.
The lyrics, ‘When I cross that line, there’s no telling how far I’ll go,’ took my breath away. That is it. We will go far. We will go all-in for this child. We will go so far the landscape of our lives, our family, our community will be forever changed. We will sail the uncharted seas and return the heart, we will be voyagers, we will venture out. Moana became a common movie and soundtrack played during my pregnancy. I was empowered to go…go far. ‘I don’t want her to suffer, we want her to be comfortable.’ These words came out of my husband’s mouth as we sat on our couch with a prenatal hospice support person, referred to us by the genetic counselor. She had already visited a few times and we really let her lead the time together. Talking about ‘different’ babies and saying goodbye soon to a child, burial gowns made from wedding gowns and talks of cold cots, donated photographers, hand molds, and keep-safe boxes.
Like a Mary Kay consultant, she unboxed items we would one day be able to have. She excitedly explained how she would be the one to bring them to us. These items would keep our child forever a part of our family. It was so sad, yet special and nurturing to have a space to talk about the baby. It was so pre-determined as ‘THE WAY’ to prepare for our child. I was not able to see what a distraction it was for us until I heard my husband and her chatting. I watched them talking. She began to share we could intervene, but this could really do ‘more harm.’ My arms crossed, I sat up a bit straighter I let the teddy bear handed to me earlier by her drop to the floor. I listened intently to their conversation. I heard the leading and probing questions, I heard the manipulation, and the uniform statements that must be said over and over to parents ‘like us’ with ‘babies like ours.’ This was the perfect time for me to update our ‘support person’ on a new path I had discovered.
At this point, the baby was moving and active, and I was learning daily online about children living with T-18. I placed a stack of papers on the table and I then interrupted their conversation, saying, ‘Actually, kids often need interventions but they can live.’ Silence followed. My husband looked at me, his eyes full of tears. I stated, ‘No more planning her death. No more preparing her siblings for her absence, and no more time wasted in grieving her, when she was alive!’ This was the day I took charge of her care. I didn’t look back, I declared for us and for her comfort, it was to never be spoken of again. The clarity and knowing were some of the greatest gifts from the lord. Resources began to find us, and I also was an eager hunter searching for what we needed. Pouncing on any and every opportunity to network, consult, share, and learn from professionals and members of the Trisomy 18 community.
‘No, not for full T-18. This was only some of what was said as we sought a surgeon for Rose. The details and comments still haunt me. But we found help! ‘I’ll take the kid.’ This was what a surgeon said who I reached out to, who had operated on a child with T-18 eleven years earlier. He agreed to take Rose on as a patient! I was thrilled, it was our first ‘acceptance’ into fair care and I was thrilled! There is a saying, ‘The hand that rocks the cradle rules the world.’ Well, with a medically complex child who is at their cradle, who is there at the most critical time to care for the medically complex newborn? Not just me! She needed a team. She needed support. She needed an intensive care unit, to be taken from the cradle and tended to. And by whose hands? I had the awesome responsibility of giving her ‘mommy by her cradle’ and handing her over to care, to rule her world.
They were essential. They were needed for her to be in this world. But my parental autonomy had to be the driving force, and they had to give her access to care. Otherwise, we would be having an empty cradle, she would have too short of time in this world without intensive care and heart repair. ‘What’s our algorithm?’ I was now very close to delivery. I found a surgeon who agreed to take Rose on. I was referred to an OBGYN to deliver Rose. She would deliver Rose close to the hospital where the surgeon was. I drove about 2 hours to meet with her. I was scared but determined to build a fair team. When I gave her my assertion of my autonomy, a stack of papers labeled ‘birth plan,’ and another labeled ‘aftercare plans,’ she looked through them. She held her head down for a moment, took a deep breath, and handed my papers back to me as she exhaled. I inhaled and held my plan in sweaty, shaking hands. They felt heavy, I felt defeated.

‘What’s our algorithm?’ she said. I was in shock, it wasn’t a ‘no.’ As her arms crossed, doors opened! There was a twinkle in her eye that lit up the room! The wheels in her mind were turning. This was the first doctor who met my fierce call to action to work for my child and fight for her life. In most cases, it could be terminal for Rose if I went silent. But now it was safe. It was safe to go silent and let her wheels turn, call in her resources and skill, and join the plan. An algorithm was put to paper. Actually put on the exam tables, explaining what they can offer! We got her to put pen to paper and use the word ‘our’! Our algorithm’ was life-saving words for Rose and a salve to my broken heart.
The first 6 weeks of Rose’s life were intense. In a system expecting her to die, they were annoyed, scared, and perplexed she was not living up to her prognosis but she was responding to the forced care and she was living.
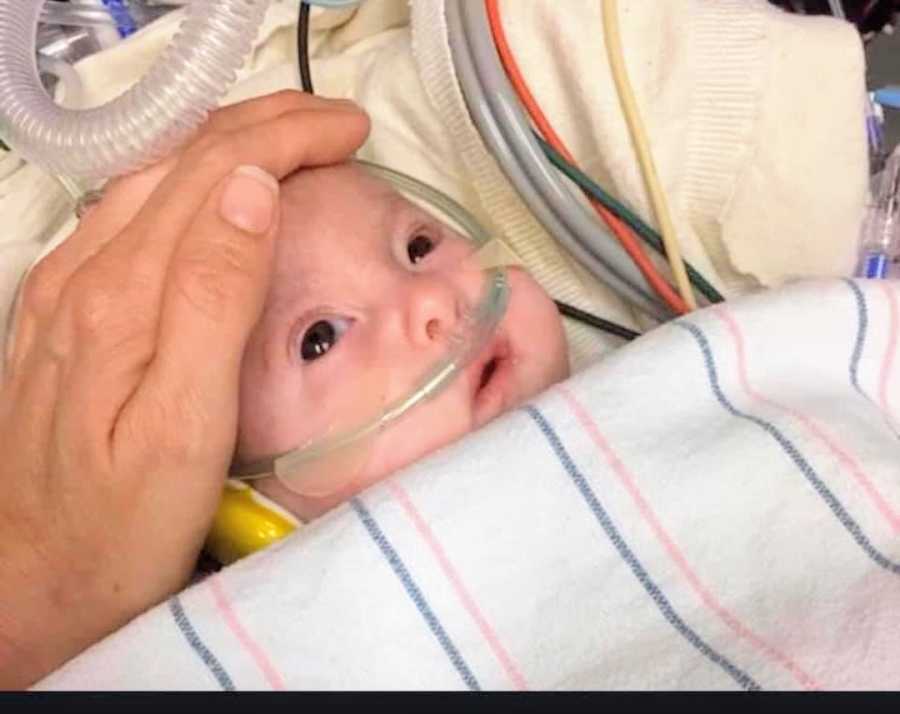
This caused panic and anger in an institution that didn’t know what to do about this girl who lived. Here are some quotes from her care in her first six weeks of life: ‘Who the f— intubated a T-18?’ ‘We will extubate when we want.’ ‘We will never re-intubate.’ ‘No one will re intubate her, not anyone.’ ‘Jaundice? You think? And you want to treat it? Why?’ ‘This is so cute you care, we will take it from her mom.’ ‘Mom, will you step outside?’ ‘Someone take mom out of the room.’ ‘No, we won’t do cath lab.’ ‘No, she can’t have a stint.’ No, she can’t have surgery.’ ‘No, you can’t talk to her surgeon.’ ‘No, you can no longer contact him.’ ‘She isn’t passing, but she is suffering.’ ‘You must take her home.’ ‘Have her watch TV at home.’ ‘Let her go.’ You are cruel.’ ‘Our established staff has an ethical dilemma in treating your child.’ ‘We don’t agree with what you are doing.’ We may need to bring in higher authority.’ ‘Think of your husband, think of your children.’ ‘We did what you asked and she is showing us she can’t live.’ ‘She drives the bus, we follow her lead. She can’t live.’ ‘Let her go.’

When Rose was about 4 weeks old, she was doing well. She had episodes that were scary and bad and did show her prognosis was poor. We were at a standstill. She held on. I refused to leave, they refused repair. I waited for repair, they waited for her to pass. We were all waiting, we were not on the same page or following the same map. Rose and I remained on a unit where we were uninvited guests. Explorers in territory not safe for us, but we remained. I was tired and alone. One night, I sat in a small hallway on a computer. I was allowed to use a computer back by the staff lounge. I began yet another email to Rose’s surgeon, knowing very well I would not get a response, but yet again I tried: another request for him to consider heart repair. I was about to head back to Rose’s room when I heard it. The ‘it’ that made all my worst fears and mistrust of her care be validated.

The charge nurse walked past Rose’s room, glanced inside, and said to the neonatologist, ‘Hey, doc,’ she did a little chuckle, stuck her hand on her hip, and said, ‘How far are we gonna go for a T-18?’ My heart sunk, my face went cold. Not hot, as it does when I passionately advocate for Rose’s needs. It went cold. I stood up and walked toward them, and I said, ‘We are going ‘far.’ Check the chart. SHE IS FULL CODE.’ I went back to Rose’s room shaking. I began to cough and I ran to the bathroom and I threw up. Disgusted and in shock to hear the papers I signed for full resuscitation, the agreement for a surgeon, and the access to the heart unit were all paper-thin plans. The access to ‘fair care’ was a facade. We were climbing higher on a house of paper-thin cards. We were getting shaken and pushed. The cards were falling, only to be later stacked against us. I guess they always were. It was just now apparent to me.

‘Slow code,’ this was the high-bred version of ‘comfort’ care. This was a facade, and what does one do with it? You can stay and play the game or walk away. With all the cards on the table and the bluffers spotted, I had no choice but to leave. To stop gambling. Keeping Rose in this care was a gamble and we had to leave. But where? I had developed a list of consults and referrals to places that offered heart repair to children with a rare trisomy. I had always included it in my care plans and info given to the hospital staff.
To be honest, I never meant to use it. I only wanted a backup plan, but never wanted to use it. We had built roots in the first 6 weeks of Rose’s Life. Living at Ronald McDonald House, finding help with my oldest children enrolled in the school there too. All six of us living in one room had become our new normal, and I didn’t want to change it, to leave my children and go farther from our normal. I also knew if she needed it we would. But why did we have to? Why couldn’t we stay and get it there? And the day came, the unit director came into Rose’s room and said, ‘Where do you want to go?’

I was in shock. One consult accepted her. Omaha, Nebraska, a lead I got from a fellow Trisomy parent. Jeannie’s daughter had flown to life-saving care a month or so earlier. She sent me information weeks earlier, telling me, ‘Y’all need to get here.’ I sent Rose’s information and even talked to Dr. Hammel weeks earlier. I told him Rose was stable. He ended the call with, ‘I would repair soon. She is at risk for hypertension, but if you and your care feel differently, I respect it. Here when you need me.’ Well, we needed him. We got accepted fast. We were denied by our insurance twice and in a 3-day haze, it was overturned by a judge and we headed to Nebraska. No one can prepare you for applying for life-saving care for your child while you await an acceptance letter and feel disappointed and unworthy with every denial. We were denied all in-state consults and a few out-of-state. Sinking and scared, Omaha reached out and we handed Rose over.

I could not fly with her, so we sent her alone. Rose was to fly alone from California to Omaha. ‘You can’t fly with her,’ I was told the day before. We moved fast. My husband and four boys and I took the night to laugh, to cry, to pack up our room at Ronald McDonald’s house, and say goodbye. My boys had never met Rose. They followed our lead their sister needed help and we all would help.

After he had dropped me off at the airport and went back to pack up our room at Ronald McDonald’s house, my husband got a call from the unit director: ‘Where’s Mom? We are about to have transport arrive. We also cleared it so her brothers can say goodbye as well.’ My husband let them know our plan. I would be in Omaha before him, and I would not be saying goodbye. Rather, I would be there on the other side to say hello.

Rose arrived in Omaha on March 22, 2018. She had full heart repair 4 days later. Thanks to Dr. Hammel and the staff of Omaha Children’s Hospital, Rose is now a happy toddler. She has a wonderful life, she has the love and support of her family, and she is an inspiration to others. We have the honor of helping her have access to fair care.”

This story was submitted to Love What Matters by Meri Willard. You can follow their journey on Instagram and Facebook. Submit your own story here, and be sure to subscribe to our free email newsletter for our best stories, and YouTube for our best videos.
Read more stories like this:
Provide beauty and strength for others. SHARE this story on Facebook with friends and family.





