“Everyone always says kids won’t starve themselves. That’s mostly true unless you have a child that will. When our youngest child, Harrison, was six months old, we started to introduce solid food. My two daughters LOVED when we started solid food and ate almost everything we offered to them, so I expected my son to be the same.
Not Just a Picky Eater
We started with rice cereal, but he didn’t seem interested. Over the next few months, we tried several different baby foods, but he did not want to eat those either. We were not too concerned. Our girls were, and still are, fantastic eaters, but we had several friends with kids who are picky eaters and figured Harrison was the same. We moved on to baby puffs, crackers, tiny bits of cooked vegetables, fruits, beans, and cheese. With no luck there, we decided to try cookies, ice cream, and other sweets. No luck.
At his one-year check-up, he had gained one ounce from his last appointment three months earlier. One.

This year of his life should have had the most physical growth, but he had not gained enough. Because he had grown in length but not much in weight, he fell off the normal range of the growth chart. His calorie intake was not supporting his growth. We were concerned, but mostly that he was going to be a very picky eater in our family of foodies.
Harrison is our youngest of three, and at this point, my daughters were old enough for soccer, ballet, and all the other activities preschoolers and elementary-school-aged kids can participate in (read: a lot of stuff). We were in the car a lot more and were sitting down all together for meals. I bought cookbooks filled with recipes for picky eaters and tricks on hiding vegetables in typical ‘kid food.’ I bought special plates and utensils I thought would make mealtime more fun. We played Yo Gabba Gabba ‘Party in my Tummy’ on repeat. If there was a product that was geared toward getting picky eaters to eat, we bought it.
Soon we started noticing he would eat chalk, paper, ice, and other non-food items, a condition called pica. We couldn’t get him to eat food, but give him a notebook and he would eat it. When each of my children turned one, I bought them Dr. Seuss’s ‘Happy Birthday to You’ book and had guests sign it. I loved looking at all the sweet comments year after year on their birthdays. Harrison found his book and ripped out the pages and ate pieces of them, destroying most of all the signatures. This was a hard part of our story for me.
Not only could I not recreate those signatures to share those memories with him one day, but I also started to fully understand Harrison’s eating (or lack thereof) wasn’t just picky eating—there was an actual problem. Mothers are supposed to be able to feed their children. It is a basic fact of life. I had so much shame in not being able to feed him, I didn’t want to admit to the pediatrician how bad the situation was. Most of the time, I would take the non-food items away from him, but there were times when I let him eat paper. I just knew he needed something in his stomach and told myself paper was better than nothing. I hated myself every single day.
Living With ARFID
When we went back to the pediatrician, he had lost a few ounces and had fallen so far behind on the growth chart, he was considered ‘failure to thrive.’ The pediatrician diagnosed him with ARFID (Avoidant Resistant Food Intake Disorder). ARFID can occur in kids with other delays or conditions, like autism, or in typical kids. As the name suggests, individuals with ARFID avoid or resist food to the point they cannot grow and develop properly, and it is not explained by another medical condition. While Harrison does have other delays, eating has always been his biggest struggle.
My child was wasting away right in front of me. You could see his ribs as well as the bones in his shoulders and arms. Blood work showed he was significantly malnourished. His low iron level was likely the culprit for the pica. Harrison was already receiving speech therapy through our state’s early intervention program, and they determined he met the criteria for feeding therapy as well. Every other week we had an occupational therapist come to our house to work with Harrison and to teach me how to get Harrison to accept pediasure as a nutritional supplement and how to start working on table food.
While I took Harrison to speech therapy and occupational therapy, my friends took their kids to ballet class and story time. After I put my kids to bed, I googled ‘nutritional value of paper.’ After my friends would put their kids to bed, they poured a glass of wine and relaxed. I felt robbed of the experiences it seemed my friends were having. I avoided taking him to birthday parties because I knew he wasn’t going to eat the cake or ice cream. I avoided going to lunch with friends because I was terrified he would grab a menu and try to eat it. I was hopeful feeding therapy would help, but after a year and a half, we were more or less in the same spot.
At this point, we were referred to an intensive feeding program, and luckily at the time, there was one at our local children’s hospital. There was a long wait list, even for the initial evaluation, but I knew this was our best shot at getting Harrison to eat enough to support his growth. After four months on the waitlist, we finally got an appointment for an evaluation. I just knew this was going to be the miracle I had been praying for. The team consisted of a GI doctor, a pediatric nurse, a child psychologist, a speech pathologist, an occupational therapist, a social worker, and a nutritionist.
They were among the best of the best in their fields. The night before the appointment, I was so excited I actually cried tears of joy. There are not many intensive feeding programs in the country, and there was one in our city. We had the best of the best right in our backyard, and we were finally going to get the help we needed.
When you have a child with any kind of special need—medical, physical, cognitive, etc.—you learn to never assume stability. You live your life standing on a fault line. There will inevitably be doctors’ appointments, IEP meetings, or therapy sessions where the ground quakes beneath you and swallows your life as you know it. You are always braced for those moments, ready to hear the difficult things, ready for the other shoe to drop. This was one of those moments for me.
Harrison was not a candidate for the feeding program, at least not at that time. He was not medically or nutritionally stable and was not something the feeding program would address. Additionally, they recommended a G tube, a surgically placed device that delivers nutrition directly to the stomach. My heart shattered.
I saw the G tube as a failure on my part. Even after over a year of feeding therapy, he was still extremely malnourished. I was determined to do whatever I needed to in order to avoid a G tube. The doctor agreed to let Harrison get monthly iron infusions to get him to a healthy level, and I would work on getting him to drink pediasure at home. If his blood work looked better and he was able to accept enough nutritional supplements, then we could avoid a G tube and they would re-evaluate him for the feeding program. There was still hope.

A Food Jag
After six months of doing iron infusions and working with a feeding therapist twice a week, Harrison was drinking pediasure and was nutritionally stable. He was officially on the waitlist for a spot in the intensive feeding program. I would love to say life unfolded perfectly after that—that Harrison drank his pediasure, went to the Intensive Feeding Program, and suddenly ate everything and we all lived happily ever after.
Unfortunately, about a month before he was set to start the program, he stopped taking the pediasure. He hit a food jag—which is when a child will eat (or in this case, drink) a few limited foods meal after meal. This causes a problem when the child decides they no longer want food or drink and they suddenly lose their source of nutrition.
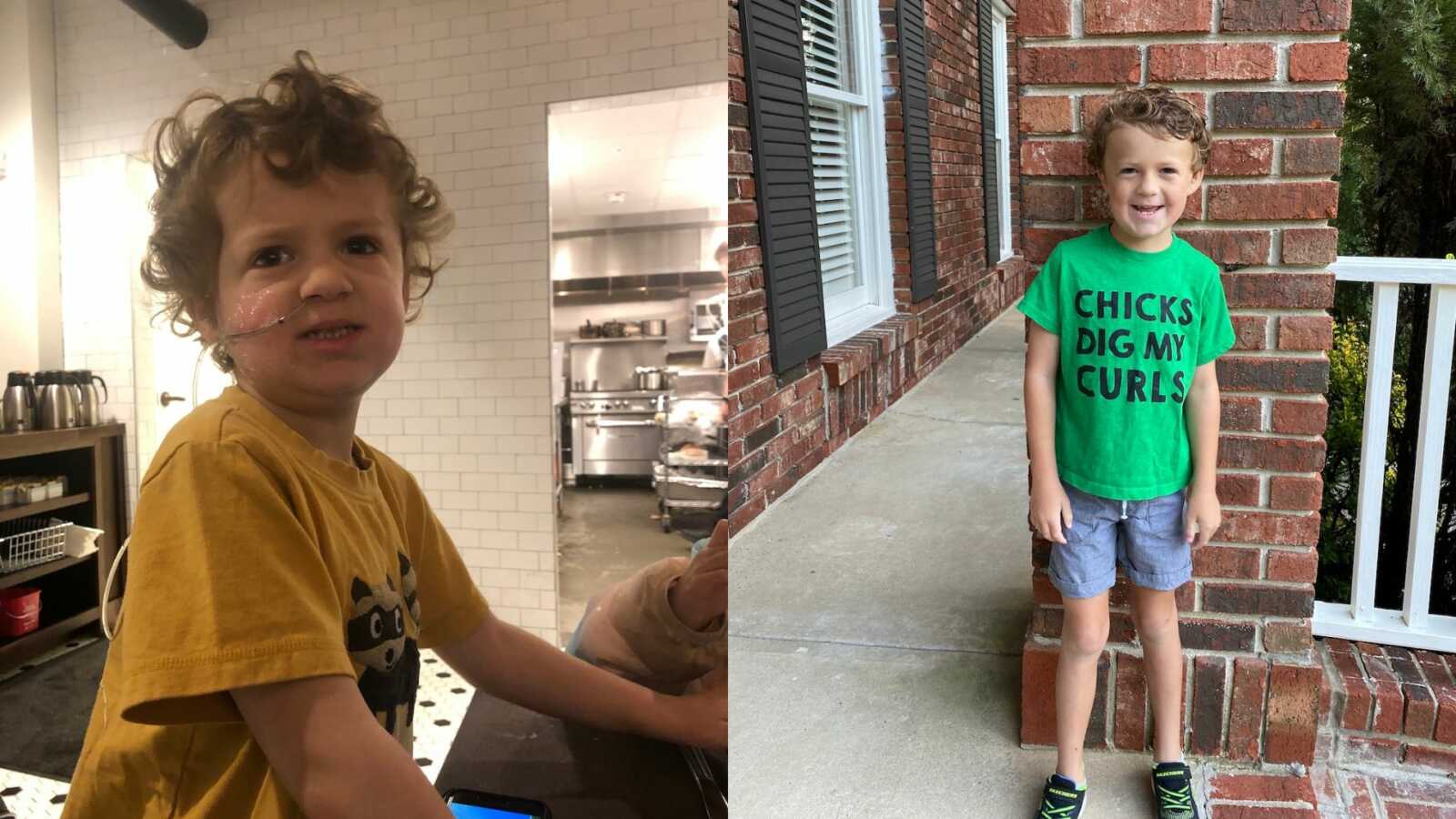
Our best option to keep Harrison on the list for the feeding program was for him to get an NG tube. An NG tube is a small tube that delivers food directly from the stomach through the nose. This was such a punch in the gut for me. At this point, I had been fighting a feeding tube for nearly two years. I couldn’t fight anymore. I just needed my child to be healthy. The day he got his tube was the day a huge weight was lifted from my shoulders. As much as I fought the tube, I finally got to see how much time I spent analyzing nutrition labels trying to calculate how much of his daily value of vitamins and minerals he was getting from the few snack foods he was eating. I knew he wasn’t going to bed hungry, he was getting nutrition each day, and I didn’t have to battle him to get it down.
Finally, we got the call we were waiting on. Harrison’s spot opened, and he would be starting the feeding program the following week. We spent every Monday through Friday from 8:30 a.m. until 4:30 p.m. at our local children’s hospital for almost ten weeks. Each day Harrison had three feeding sessions. The treatment rooms were equipped with a camera, and I was able to watch from a viewing room that played the live feed of the session. At the beginning, Harrison fought the therapists and refused the food. He cried. He yelled. He pleaded for them to stop. It was like watching people torture my child. I would constantly question whether we had made the right decision for Harrison. The days were long and emotionally draining.

I spent most of the days either crying or feeling so defeated. I spent eight hours a day watching my child struggle. During a meeting with the program director, she looked right at me and said, ‘Harrison isn’t broken. There is nothing to fix. This is a part of him. It’s not what you expected, but it’s not bad or wrong.’ Learning to live by this truth is my work. Learning to eat enough food to survive is Harrison’s work. I had to learn that the disappointment, worry, and sadness are always going to be a part of our story. But throughout those ten weeks, I saw the progress, hope, and amazing people that were helping my child eat are also a part of our story.
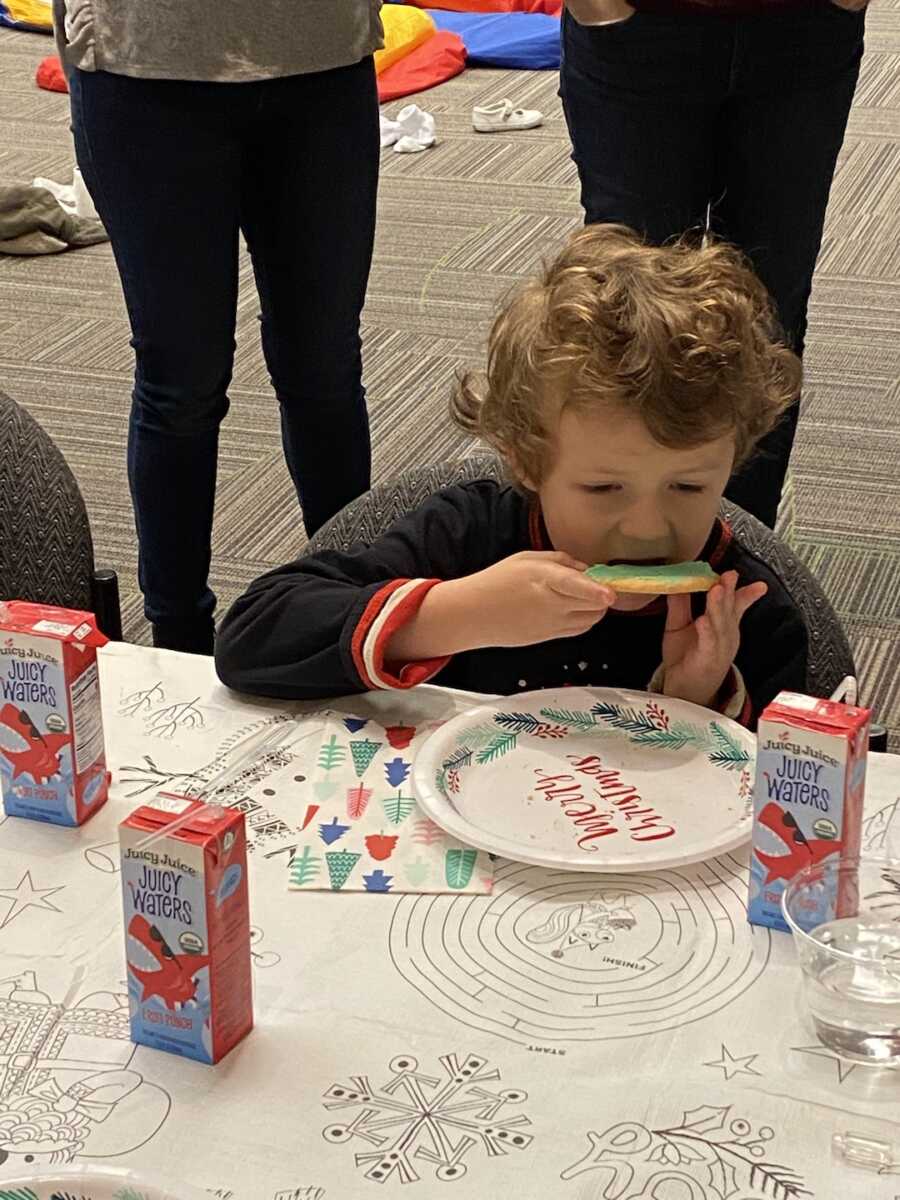
After a few weeks, Harrison had learned the routine and stopped fighting as much. He started to accept pediasure. A few weeks after, he had his first bite of yogurt. When he graduated the program, he was NG tube free, would drink enough pediasure to be nutritionally stable, and would eat yogurt and pureed sweet potatoes. He left with three wins. I left with the road map for introducing new foods and the confidence I could, in fact, feed my child. The next year was even more difficult than the 10 weeks in the program. My husband and I were responsible for all the preparing, measuring, and feeding. We didn’t have a team of therapists and doctors living in our house to do those things.
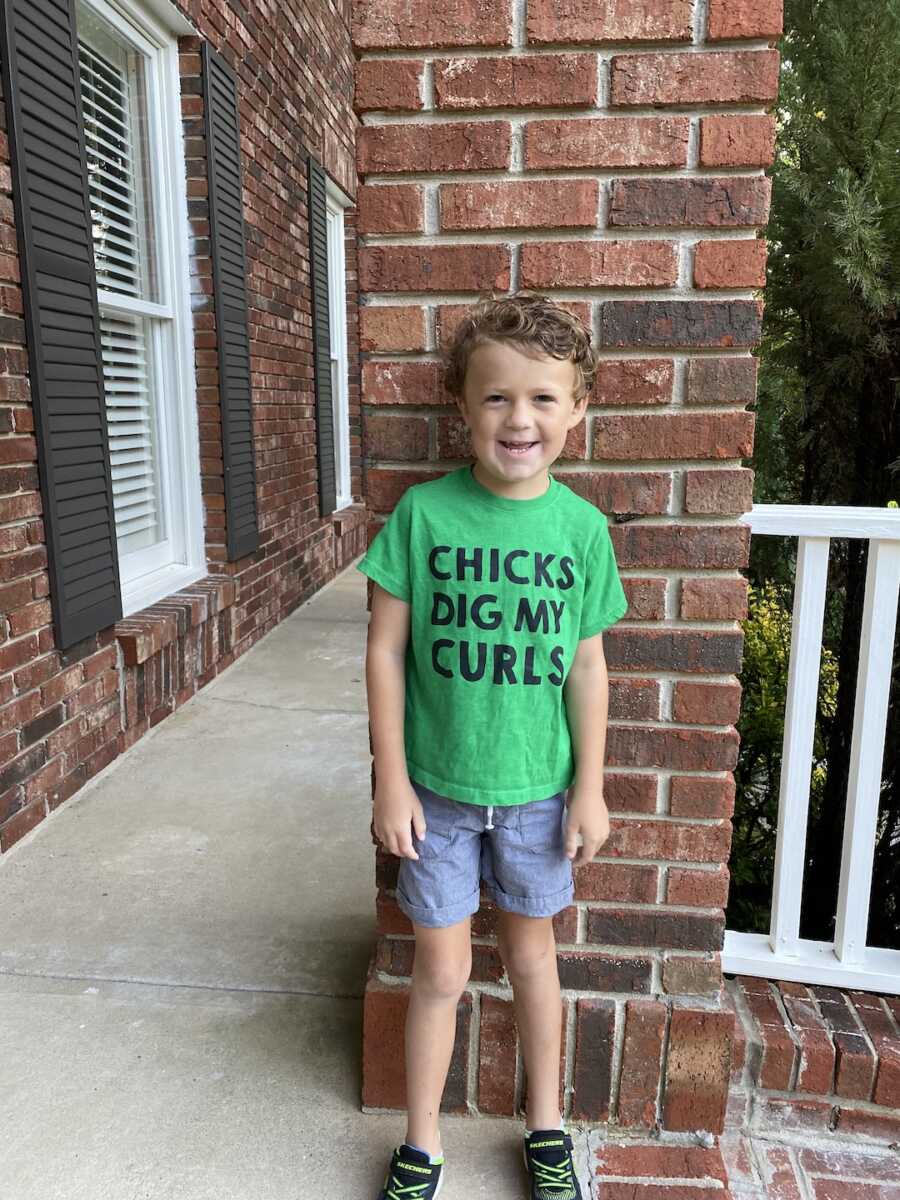
But, in that year, we introduced 27 new pureed foods and were able to transition most of those foods to their table food counterpart. He still struggles with eating fruits and vegetables, and we still use an intentional feeding protocol to introduce those foods into his meals, but he has come a long way. We have all come a long way. Harrison still requires extra attention at school during lunch to make sure he is eating his food. He still drinks pediasure for supplemental nutrition. We still must check the menu before we go to restaurants before we go to make sure there is something he can eat. I used to see those things as negatives and things that made him stick out as ‘different.’ Now I see them as important steps to keeping him healthy. If he needed medicine, I would have no problem giving it to him.
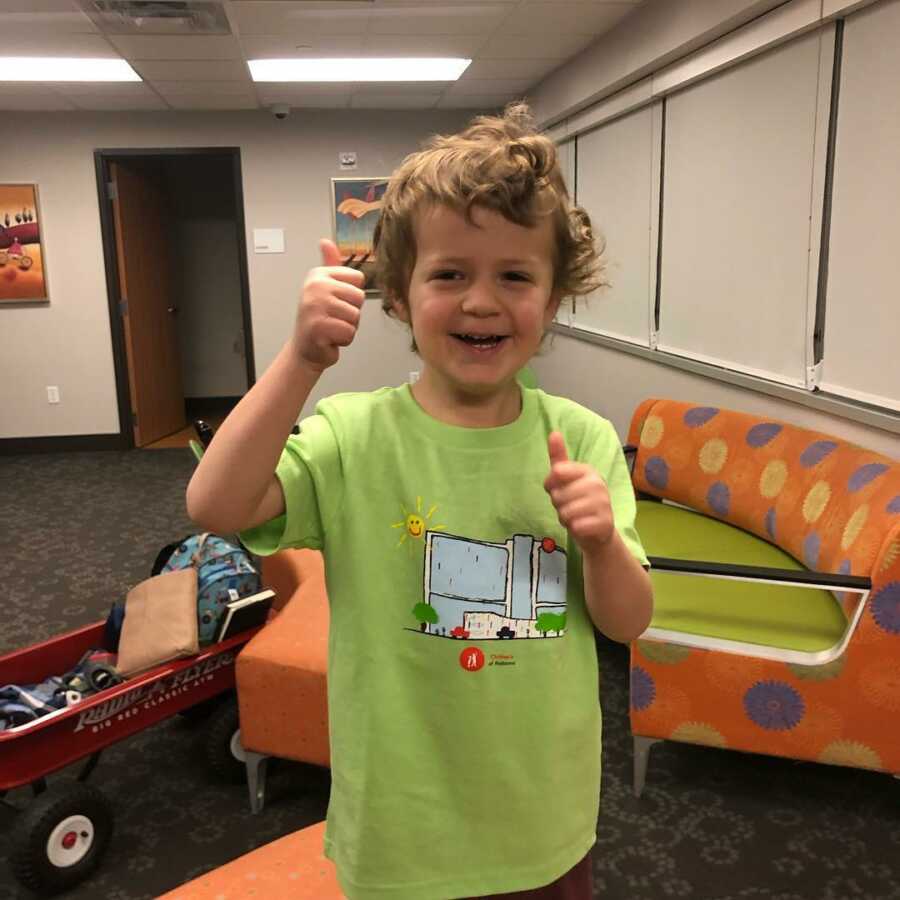
For Harrison, monitored eating and pediasure are his medicine. We don’t take eating for granted. Will my child always struggle with eating? Probably. Will we find a way to support him and keep him healthy? Yes, because we have the tools to know what to do, and we have an amazing village to ask for help when we don’t. ARFID is not easy, but it’s a part of Harrison. And the program director was right, he’s not broken, there is nothing to fix. There’s just a little more to work on when it comes to eating. He’s worth it.”
This story was submitted to Love What Matters by Emily Israel of Birmingham, Alabama. Submit your own story here, and be sure to subscribe to our free email newsletter for our best stories, and YouTube for our best videos.
Read more stories like this:
7 Feeding Tips For Your Autistic Child With Sensory Aversions
Do you know someone who could benefit from this story? SHARE this story on Facebook to let others know a community of support is available.