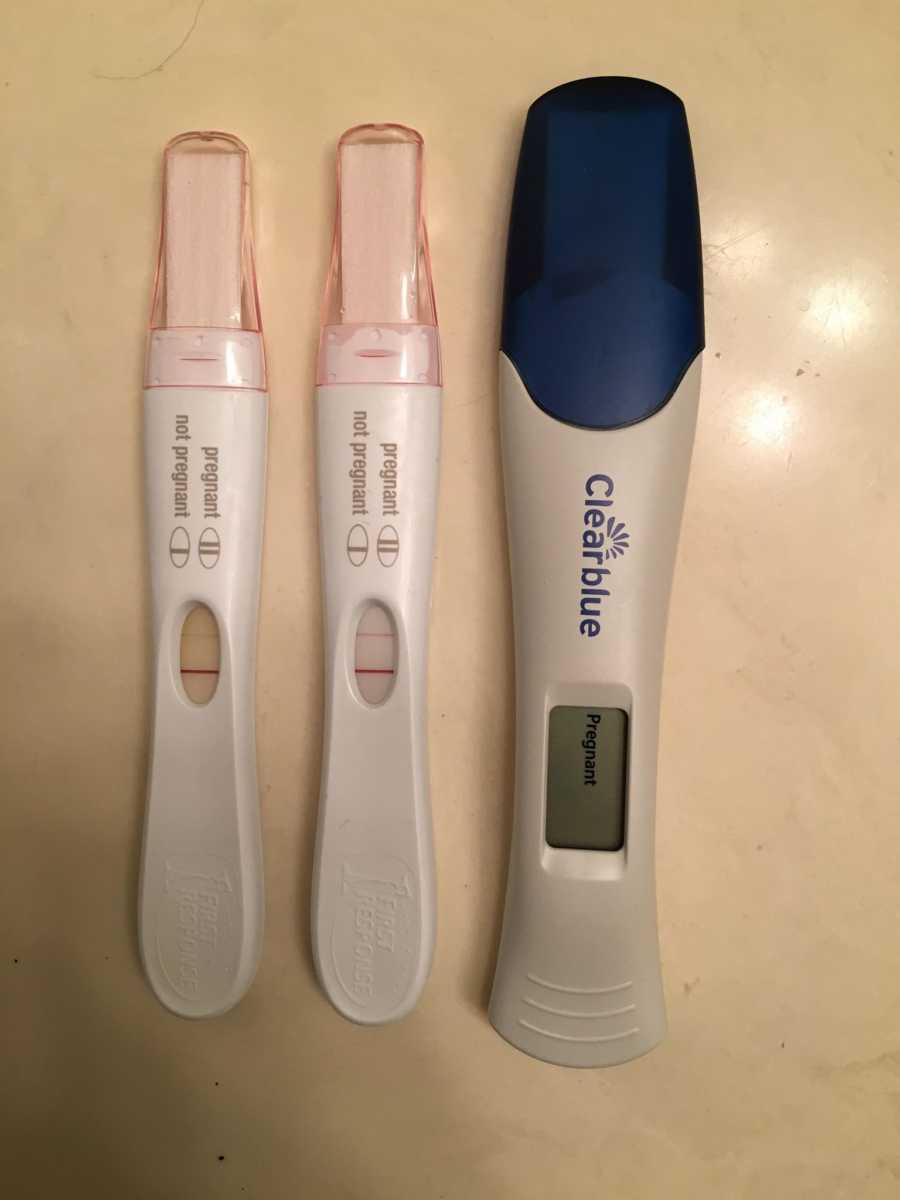
“It took us a little while to get pregnant. Luckily, we were the first of our friends to start trying. I wasn’t constantly slapped in the face with pregnancy announcements and for that I am grateful. There is a history of PCOS in my family and I wasn’t spared. It took several combinations of medications to get us there in a little over a year with no shortage of tears and frustrations. On March 8, 2018, I got the faintest positive on a pregnancy test. A few days later my beta levels were almost double what they typically are supposed to be. A week later we went in for an ultrasound and our nurse gave us the shock of our lives: twins. We were elated, but she told us to hold off on our joy as Baby B’s sac was measuring very small, which often leads to reabsorption or a ‘vanishing twin.’ We immediately called our parents one-by-one and told them our incredible news, but held off until 12 weeks to tell all of our friends and social media. I was due on November 28th, we had plenty of time to tell the world.

My pregnancy was not an easy one. I vomited multiple times a day for pretty much the entire time. At 11 and 13 weeks I bled abundantly, both times assuming I was miscarrying. They could never find the origin of the blood and both babies continued to grow, though Baby B lagging slightly behind in size and heartbeat strength. Pat and I would often leave appointments joking ‘dammit Baby B!,’ partially to prepare her for a lifetime of playful comparison, and partially to protect ourselves if something ever happened. Despite my morning sickness and bleeding, we went into our 20-week anatomy scan assuming that things were perfectly fine. They weren’t.
We could tell during the scan that there were two heartbeats, four arms, four legs, two adorable little noses. After the scan, we were told they were both measuring on the small side, and that we’d need a follow-up scan the next week with Maternal Fetal Medicine. I asked my doctor if we should be panicking and he assured me that he’s referring us ‘just to be safe.’ The following week, after our scan, we were taken into a patient room to speak with the MFM. She explained to us that both of our girls, our tiny little-nosed girls, had inconsistent blood flow to their placentas. They were growing much slower than expected and not receiving what they needed from me. They were diagnosed with intrauterine growth restriction (IUGR) from intermittent absent-end diastolic flow, a condition that the MFM said she rarely saw this early. The course of this diagnosis typically results in early delivery, but I was just barely 21 weeks along. The MFM said our new goal was to get to viability, 25 weeks, and the likelihood of one or both girls reaching viability was approximately 50%. I was instructed to drink a ton of water, eat protein, and return for weekly Doppler scans to monitor blood flow. When the blood flow was determined to have stopped or reversed, I would be admitted and the girls would be delivered as long as we reached 25 weeks or the girls measured around 500g (1lb). We were devastated and, in hindsight, had absolutely no idea what delivering a 25-weeker meant, nor did we think about the complications that come with a baby born that small. I made a paper chain to count our time and together we waited, making hopeful plans for our family of four, as the days slowly crawled by.

At 23+4 my blood pressure spiked and I was briefly admitted. We had our weekly Doppler and the MFM came again to share the details with us. This time, our strong baby A was showing signs of oligiohydraminos (low amniotic fluid) and further growth restriction, measuring in the 3rd percentile, only 340 grams. Baby B was measuring in the 14th percentile and their roles had switched – her blood flow was a bit stronger and she continued to grow ever so slightly, measuring 420 grams. Neither baby was viable. I was discharged from the hospital and we met with a neonatologist who matter-of-factly told us if I could get them to 24 weeks, he would do everything he can to try to save them.
The following week, on August 8th we returned for another Doppler. The ultrasound techs were usually talkative and cheery during the scan, but this tech was silent. Pat held my hand and we waited patiently as she scanned each leg, arm, little nose. After about a half hour, we heard exactly what we were mortified to hear; ‘I’m so sorry, there’s no heartbeat.’ Baby A, our strong, beautiful twin, had passed some time in the five days between my admission and the scan. Baby B’s blood flow had reversed, which we were told was very dangerous, and I was immediately admitted for monitoring. I was given steroids and magnesium to give her strength, and the plan was to give her a few days to gain the effects, but we had to be diligent to watch for signs of distress and deliver as soon as possible if she went into distress.
Because of the cord flow issues, she was not yet considered viable. The neonatologist came to visit again and told us she had to be around 500 grams to be intubated…so we were prepared that given her measurements at the last scan, that her shot at life was about 5%. A five percent chance that my one surviving, beautiful little nose would see this life.
My parents rushed down and together we spent Wednesday through Saturday crying and staring nonstop at her heart rate monitor, hoping she’d be big enough to intubate and live. The nurses who cared for us were so incredibly sweet, but clearly walking on eggshells around us. One in particular wept as she took my vitals.
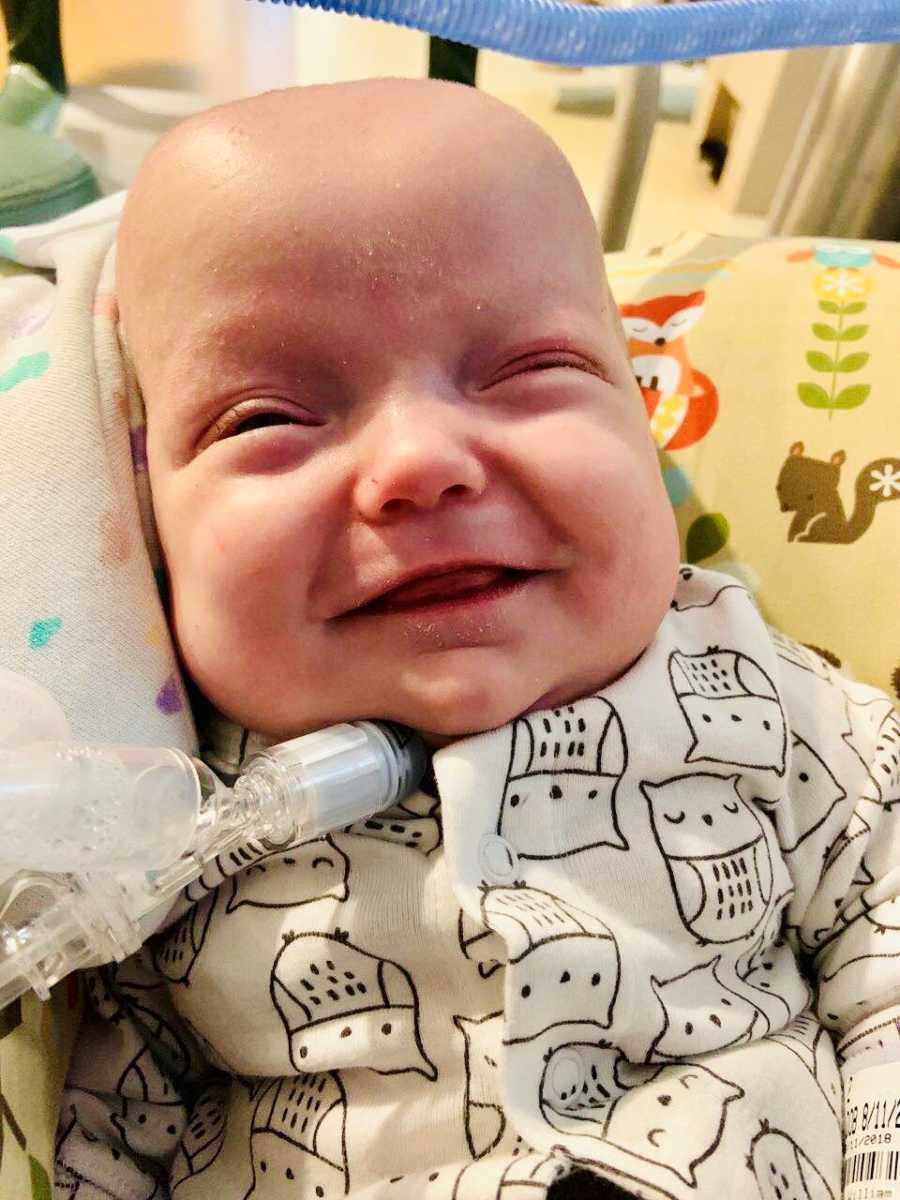
On the morning of Saturday, August 11, I went into a c-section and first delivered our beautiful Baby A, and then the loudest, feistiest 504-gram baby girl the NICU team had ever seen. We named her Lily Margaret after my aunt and Pat’s grandma. My aunt is the glue that keeps my dad’s family together, and Lily will do just that for us, no matter the outcome. Surprisingly, Lily didn’t need to be intubated immediately. She breathed on her own for about an hour and a half and was literally screaming at the nurses for some time before heading down to the NICU. When the neonatologist explained to us that there was a 5% chance she would survive, we didn’t know the road we’d travel down to get past ‘surviving’ and make it to ‘thriving.’



We spent 256 days in the NICU. 256 days filled with uncertainty, sadness, fear, and anger, but also moments of sheer beauty and joy; her first bath, first clothes, first bottle, holidays, and development of friendships that will last forever. We learned to lean on one another in way we never thought possible, and looked to the strength of our friends and family to help us just survive from day to day. When Lily was one month old, she had an exploratory bowel surgery because she had not pooped since she was born. It took weeks of enemas, contrast studies, and medications to arrive at the decision to operate. At the time, we had absolutely no idea how risky it was to operate on a 1lb baby. Her heart stopped (‘coded’) on the operating table and she was brought back to life, but we were so blinded by everything going on, that the magnitude of this surgery took months to process. The week after surgery we almost lost her again. Her lungs had become increasingly damaged by the ventilator that was keeping her alive, so much so that she maxed out the support that the vent could provide. The team put her on a high frequency oscillating ventilator for a week, to help deliver pressure support that she needed, but with the hopes she’d ultimately require less support. This week was extremely difficult as we were, yet again, briefed that she may not make it. I did lots of research on other treatments, and the team agreed to trial low-dose steroids to help her lungs grow in a short amount of time. She responded well to the steroids and was able to return to the traditional ventilator.


As a result of her first surgery, her small intestine was disconnected and she had an ostomy for three months; a section of her intestine was pulled through her stomach and the rest of her intestines were left to rest and grow. In December she had her bowels reconnected and she lost minimal bowel – it is truly amazing that we’ll have no long-term gut issues. This is our biggest victory in that all she will have is a gorgeous abdominal scar to show for months of pooping out of her belly.
We worked for months on extubation to CPAP from the endotracheal tube and we were ultimately unable to extubate her without serious repercussions, such as dangerously high CO2 and apneic episodes. Some of these episodes resulted in resuscitation- seeing my child turn blue and require chest compressions is something I wouldn’t wish on anyone. She had been ventilated for so long and her little lungs were so scarred and damaged. In January, after nearly 5 months of being unable to extubate, Lily had a tracheotomy to create a semi-permanent hole in her trachea to help her breathe. She has a trach tube down her trachea, secured around her neck, and connected to the vent. Before the trach, she had to be sedated so that she wouldn’t rip her tube out, so now that she has this more stable airway, we can begin working on all of the milestones she missed while she was very sick. During this surgery, she also had a gtube placed for us to use while we work on introducing oral feeds.


The decision for a tracheotomy was not an easy one for us as it requires around the clock eyes on Lily because the trach can occlude or pop out, making her unable to breathe. We have gone through incredibly extensive training in order to care for her, and we have nursing care in our home 3-4 days per week (we’re entitled to 12 hours a day but there is a nationwide home health nursing shortage). We are lucky that several of our NICU nurses, now dear friends, are providing our in-home nursing. While the medical side of this has been extremely scary, the trach is allowing her to do things we always knew were in there- she can now hold her head up, she can track movement, grab, laugh (silently), smile, roll, we’re working on tummy time, and just started bottle feeding. She’s been evaluated by neurologists and developmental pediatricians who feel that with time she will catch up and shouldn’t have many long-term developmental needs. We were very concerned about cerebral palsy and long term effects of sedation (she was on fentanyl/morphine/methadone for 5 months), but there seems to be minimal research to suggest that she will have these needs if she is not already showing signs.


We have weekly speech therapy, physical therapy, developmental therapy, and occupational therapy. She has monthly pulmonology appointments to evaluate her lung maturation. The pulmonologist suspects she’ll be vented for another year or two, then ‘capped’ for a year (not connected to the vent but the trach stays in to provide a stable airway to prove that she can breathe on her own). The goal is total decannulation by kindergarten, if not sooner. She’ll have intensive speech and feeding therapies because the trach makes it very difficult to speak and eat, but we’ll learn. I can’t wait to hear her really cry one day.



This has been the most difficult nine months we could have ever imagined, but we walked out of the NICU with our living miracle. This chapter tested our marriage, love for one another, and taught us that we can rely on our amazing family, friends, and hospital staff who became family. Severe chronic lung disease, a bowel perforation, 3 surgeries, 5 life-threatening infections, 4 code/total resuscitations, sedatives, paralytics, 1 MRI, 7 echocardiograms, 150+ x-rays, and millions of dollars later, we’re finally home. And I get to spend each day with the most amazing 14-pound child imaginable. Dammit, Baby B.”

This story was submitted to Love What Matters by Jessica Wolff of Illinois. You can follow Lily’s journey on Instagram. Do you have a similar experience? We’d like to hear your important journey. Submit your own story here, and be sure to subscribe to our free email newsletter for our best stories.
Read more compelling stories of children fighting rare conditions:
Do you know someone who could benefit from this story? SHARE this story on Facebook with your friends and family.



