Early Signs And Diagnosis
“I knew something was ‘not right’ when I first started my period in high school, as I struggled with intense cramping that led to nausea, lightheadedness, and hot flashes. I tried my best to supplement with heating pads, Tylenol, and exercise. But some days, I would have to take the L and lay in bed until I slept off the pain. I would miss soccer games or hangouts with friends because of the intense cramping I was having during my period.

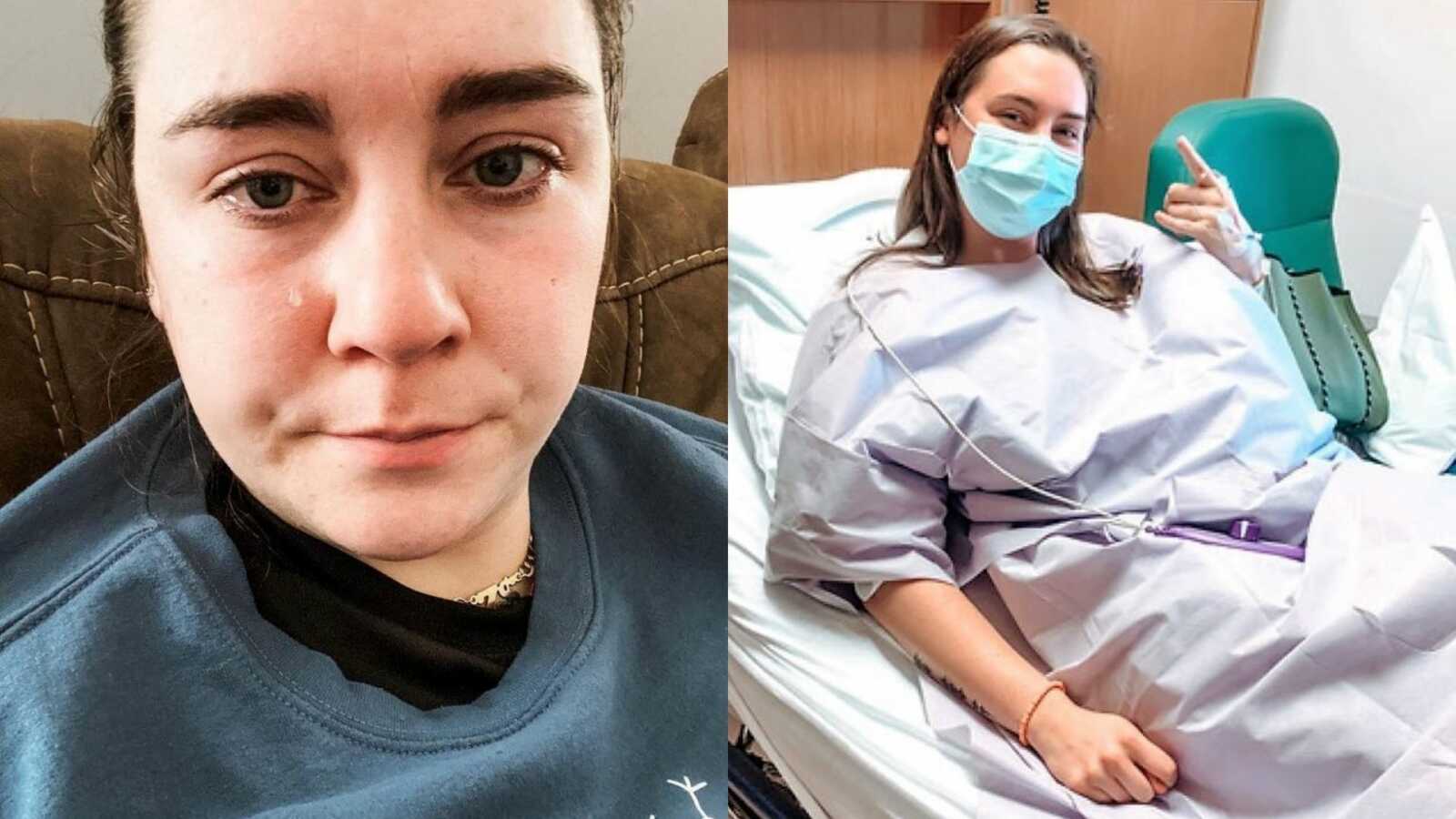
I continued to notice something was not right when I became sexually active and the pain was excruciating during those experiences, not just on my period. At the time, I thought it was normal. It didn’t help I was with a horrible guy who cared more about finishing than my pain and discomfort. I have vivid memories of crying for every intimate moment to be over because I was hurting so bad. It took me opening up about the relationship to realize pain with intimacy/sex is not normal, and to pursue further treatment.
After seeing 2 different OBGYNs who cared more about making sure I was on birth control than addressing the root of the problem, I finally found a doctor who would listen to me. I underwent laparoscopic ablation surgery in 2014, which officially diagnosed me with endometriosis. This diagnosis came approximately 7 years after my symptoms started, which is the average number of years it takes for a woman to get diagnosed with endometriosis.

I was definitely nervous about surgery, but I don’t think I realized at the time what implications came along with an endometriosis diagnosis. I was just happy to know what was wrong. Thankfully, I found significant relief from my symptoms for a few years, aside from the usual discomfort during periods.

Flare Ups
Around 2018, I started to have problems again—more significant pain all month long, GI issues, bloating, and mental health concerns. Pain with intimacy was back and I was bleeding irregularly and passing quarter-sized clots following intimate experiences. The pain would feel like a fire-lit icepick stabbing into my ovary, pelvis, and stomach, which would have me doubled over in pain.
I work as an occupational therapist, and at the time I was working full time in the hospital. There would be moments out of nowhere when I would have to sit down at a computer in the hallway and fold over onto the counter because the pain was so significant. I worked all day with patients who were in pain while pretending I wasn’t experiencing 6, 7, 8/10 pain as well.

The GI symptoms began to impact my ability to complete my work as well because the pain was not only in my reproductive organs but my stomach and intestines too. Once I realized this was impacting my quality of life as well, I sought out a gastroenterologist. In 2020, I had a colonoscopy/EGD where I was diagnosed with IBS, which is commonly diagnosed alongside endometriosis. The IBS diagnosis didn’t really provide me any peace of mind or ease of symptoms.

Unfortunately, this doctor mainly recommended I clean up my diet and exercise more if I want to feel better. Meanwhile, I was working out 5-6 days a week, working on my feet all day long, and eating fairly healthy. I ended up having an emergent cholecystectomy in March of 2020. However, I did not experience GI relief. I was desperate to feel better. I was so tired of getting sick after every meal, or right when I woke up when I hadn’t eaten. Literally any time my intestines would attack.

I tried elimination diets, no gluten, no dairy, low fodmap, whole30 – you name it. I couldn’t identify any food-based trigger for my GI discomfort. I sought out a new OBGYN in my city as my previous doctor who did my surgery was retiring. Unfortunately, I was disregarded by this doctor. She immediately recommended I take a form of birth control that is found to have terrible side effects and is very similar to a chemotherapy drug. She also recommended a hysterectomy, which DOES NOT cure or fix endometriosis-related pain.
Endometrial Excision
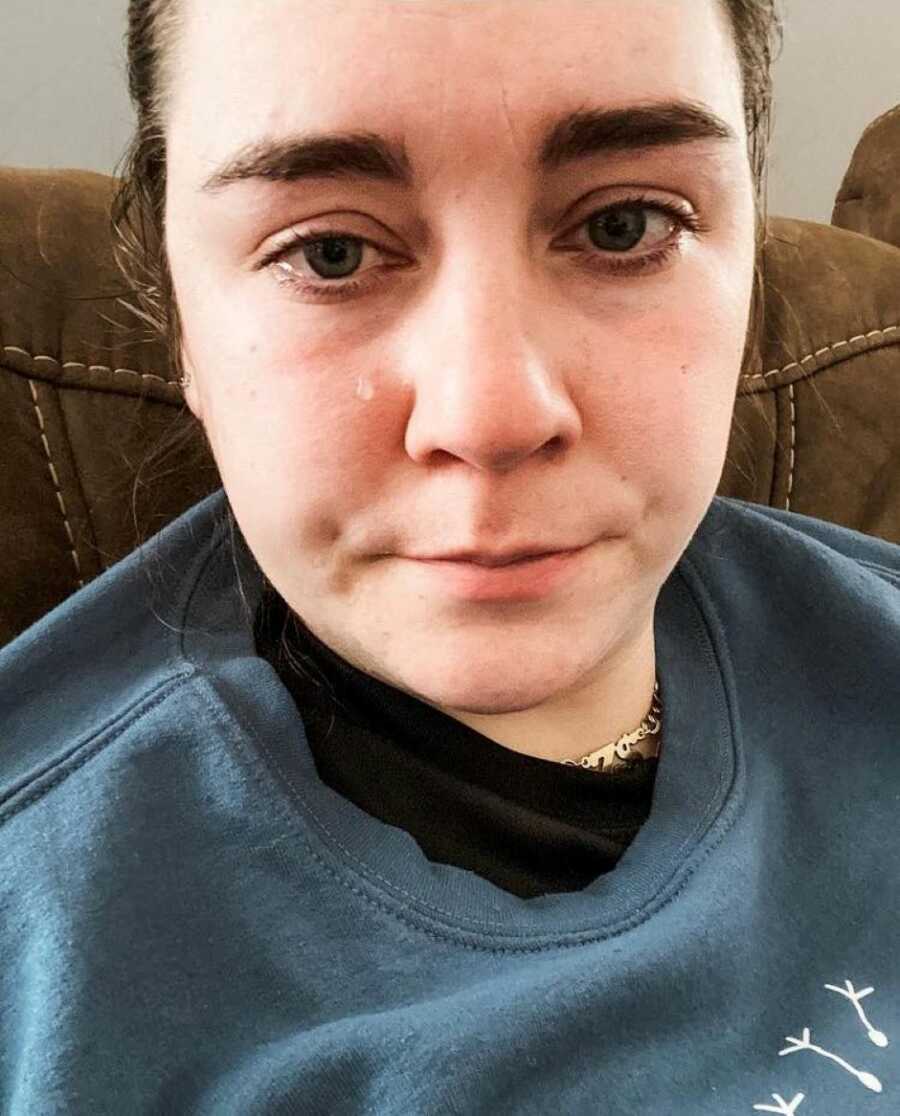
Despite advocating for myself and continually endorsing that my endo was back and stronger than before, I was written off by that doctor. I did some research and found a reproductive endocrinologist who is versed in endometriosis and heard my story and agreed to do surgery again. In Dec of 2020, I had another surgery for my endo. However, this doctor performed endometrial excision—where they completely cut out all signs of endometriosis.

It was found on both ovaries, my anterior and posterior pelvic cul-de-sac, my bowel, and my appendix (which was removed). I went into this surgery more nervous and frustrated knowing that although he may be able to remove the endometriosis, I knew it would come back. It was only a matter of time. Things were great for a while after recovery, as I was on a new medication proven to alleviate endometriosis symptoms (Orilissa).

What I didn’t know was how significant the side effects of this medication would be. Decreased bone mineral density, menopause symptoms (weight gain, hot flashes, night sweats, hair loss), and suicidal thoughts. For a while, I dealt with the side effects because my endo pain was non-existent. I wasn’t bleeding at all, and I was able to live my life more normally. After about 10 months on this medication, the suicidal ideation and dark thoughts became increasingly more significant and scary.
I reached out to my doctor, who had me stop the medication immediately and connected me with a psychiatrist. Thankfully, those symptoms eased fairly quickly after coming off of that medication. But the frustration, depression, and anxiety remained. Unfortunately, the weight of living with endometriosis causes intense anxiety and depression. I have PTSD from medical trauma and previous sexual relationships.
Anxiety And Depression
Depression from grieving the old life you had when you were pain-free or blissfully unaware of what the future might hold. Another side of the depression is grieving the life you could have had, the events you could have attended if you weren’t in pain, and the enjoyment of different events you did attend but were too busy in pain/thinking about the pain to even remember what happened.
The anxiety of anticipating an important event and wondering if your body will decide to revolt. Anxiety of losing friends for canceling yet another set of plans. Anxiety that you are a burden to your significant other, family, and friends. Anxiety that you annoy your doctor by sending them messages with more concerns, new pain locations, and new symptoms.
Advocacy And Awareness
I wish I knew what getting diagnosed with endometriosis back in 2014 meant. I didn’t know it meant chronic pain, significant bloating to the point I look 6+ months pregnant, chronic fatigue, concern for infertility, and no cure. If someone tells you they know the cure for endometriosis, they’re lying. I wish people on the outside knew there are so many illnesses and disabilities that are invisible.
I work a full-time job as an occupational therapist, coach soccer, and work out multiple times a week. I may not look sick, but on the inside, it’s a different story. Studies say endometriosis is one of the top 20 most painful conditions, yet treatment for it isn’t accessible. Many excision specialists aren’t able to take insurance and require out-of-pocket pay.

Pelvic floor physical therapy and other forms of treatment (cupping, acupuncture, pain management, functional medicine) are not covered by insurance. It’s a shame that 1 in 10 women are basically set up to be in excruciating pain without effective treatment and support, and that’s just how it is.”


This story was submitted to Love What Matters by Zada H. from South Carolina. You can follow her journey on Instagram. Submit your own story here, and be sure to subscribe to our free email newsletter for our best stories, and YouTube for our best videos.
Read more stories from endometriosis warriors:
Please SHARE this article with your friends and family to raise awareness about endometriosis!