“July 12, 2017. The day my life changed. I learned from a doctor I had not one, not two, but three rare diseases. I was diagnosed with Budd-Chiari Syndrome, Paroxysmal Nocturnal Hemoglobinuria (PNH), and Polycythemia Vera. A rare liver disease and two rare blood diseases.
A 30-year-old healthy, young woman ready to embrace a new decade and start her family—that was me and my plans for 2017. I had just turned 30 years old, an age I was looking forward to and had just celebrated my birthday on a cruise with friends. I hesitantly said goodbye to my twenties and looked forward to my thirties with hope and a new maturity on life. But being 30 for me, as I was going to quickly find out, would have a whole other meaning.

Growing up, my visits to the doctor were few and far between. Most people only go to the doctor when sick or to complete an annual preventive exam – and such was the case for me, up until August 2016. Today, I find myself in a doctor’s office at least every other week.
My diagnoses were a bittersweet answer to an 11-month question mark. To make a very long story short, my journey started with what was originally thought to be a dysfunctional gallbladder. I started having various symptoms around August 2016, and after undergoing just about every test and scan medically available, it seemed my gallbladder was at fault. But after having my gallbladder removed in October 2016 and realizing there was still something going on with my body, my medical witch hunt began.

Here is the simplest, fastest timeline of my diagnoses (try to hang with me here): Blood clots in my liver were the first things to be found. This led to being diagnosed with Budd-Chiari Syndrome. Then, blood tests revealed I also had PNH and Polycythemia Vera. It all started to make sense, after researching that both of these blood conditions can cause the liver condition named Budd-Chiari Syndrome. Now, let me unpack this.
I started out with a gastroenterologist (stomach) and hepatologist (liver) and ended up finding myself in an oncologist (cancer) and hematologist (blood) office. The doctors just couldn’t figure out why my blood levels were so abnormal. Interestingly enough, two simple, but rare blood tests—after months of numerous procedures, scans and hundreds of other blood tests—finally showed I was a rare case indeed.
I remember I diagnosed myself with Budd-Chiari Syndrome. I was researching anything and everything, and I came across this disease. I thought I was being ridiculous when I went to ask my doctor if that disease was possibly what I had, but I knew I had to ask the doctor anyway to make sure we weren’t leaving any stone unturned. When my doctor’s response was, ‘Yes, that’s exactly what you have,’ you can imagine how taken aback and surprised I was. Budd-Chiari Syndrome is an extremely rare condition where your hepatic (liver) veins are constricted, so the flow in and out of your liver is affected. For me, I had blood clots in those hepatic veins and it created scarring, congestion and portal hypertension (high pressure in a main liver vein).
Paroxysmal Nocturnal Hemoglobinuria (PNH) is a chronic, acquired (not hereditary) disease of the bone marrow. A mutated stem cell produces abnormal red blood cells that lack two protective proteins; the blood’s immune system, known as the complement system, then destroys those abnormal cells. This destruction process, known as hemolysis, is what wreaks havoc on the body through blood clots and other complications and causes this disorder to become life-threatening if not caught and treated. PNH affects 8,000-10,000 people in North America and Europe, with only 400-500 cases diagnosed in the United States every year. This equates to about 1-5 people per million of the population! PNH is unpredictable and is very much an individualized disease, meaning each person can have different symptoms, outcomes, or quality of life. Between May and July 2017, I had suffered severe liver damage due to clots in the liver and had also developed a clot in my head. Interestingly enough, those are the two most common areas for blood clots with PNH: the liver and the head.

Polycythemia Vera is ironically the exact opposite problem in the blood from PNH. PNH kills off red blood cells, and because of that, anemia is a very common issue with PNH patients. But Polycythemia Vera is a condition in which your stem cells create too many red blood cells. You have too much blood essentially, which is also a blood clot risk. For me, my issue is not anemia, as it is with most PNH patients. It is that I have too thick of blood. Also, weirdly enough, these two blood diseases counteract each other. As the PNH drops my red blood cell levels, the Polycythemia Vera creates too many cells; they oddly level out my blood. Polycythemia Vera is also extremely rare, especially in those around my age. This disease is mostly found in older adults in their 50s and 60s. So, again, I am a very rare case.
Rare diseases are often times not found because they are so hard to diagnose. The symptoms I had early on were very general symptoms that did not point specifically to the original issue: vomiting and dry-heaving, gastrointestinal issues, feeling overly exhausted (to the point I thought I was experiencing depression). Those are not very specific symptoms that point to any one disease. Also, these diseases are not common. In fact, for me, I am even more rare because I have had all three diseases at the same time. It is extremely rare to have both PNH and Polycythemia Vera, because they are opposite problems in the stem cells. And none of these diseases are passed down hereditarily. They are all randomly acquired and not inherited. And no one really knows why or how you get them.
So now that you know the gist of my diseases, let me take you back to the beginning. On July 11, 2017, I was sitting in front of a doctor being told I would need a liver transplant within a few months. A month before, I had a MRI done and it showed the blood clots in the liver. The Budd-Chiari Syndrome was the first disease we found. To say I was shocked would be an understatement. But then, 24 hours later, I received a phone call from the same doctor, telling me I also had PNH, which definitely changed things up. Because PNH can cause blood clots in the liver (and ultimately cause Budd-Chiari Syndrome), the plan was then changed to treat the blood issue so damage to the liver would stop. The dots were starting to be connected, and we learned the PNH was the origin of everything going on. The symptoms I was experiencing were results from liver damage, as well as blood abnormalities, all originating from my PNH.
Only time would tell if a liver transplant would really be needed. Your liver is a remarkable organ and can regenerate itself over time. With any major disease, time is of the essence, so I started an infusion treatment for PNH with a drug called Soliris less than a month after I was diagnosed. Soliris is one of the treatments for PNH today and allows for a better quality of life with PNH, making a normal, prolonged life possible. (It is a life-long treatment for PNH, so I go into a facility to receive the IV infusion every two weeks). When I started Soliris, we were waiting to see if my liver would heal. Sadly, after about two years and hospital visits every other month, it was apparent my liver was too far gone and was never coming back. A liver transplant was imminent. The ongoing damage to the liver was stopped, but the damage from the initial blood clots was too great.
I went through a transplant evaluation at the Medical University of South Carolina in Charleston, SC in March 2019. It was an exhausting, long, 12-hour day of numerous tests, being poked and prodded, and talking with the transplant team. After four more months of checking off all the necessary requirements to be listed, I was put on the UNOS waiting list for an organ in July 2019. Four months later, in November 2019, I would have my liver transplant.
It was 9:00 a.m. on Thanksgiving Eve, November 27, 2019. My phone rang. I saw the area code and immediately knew this was it. So many days and months of preparing, talking things through with my husband and family, trying to wrap my head around this reality mentally… and still, nothing could have prepared me for that day. It was time.
I wasn’t terrified. I was ready, but of course still scared. And more than anything, shocked. When I think back on that day, it’s just a huge blur. I remember bits and pieces, but the hours of the day fly by in my memories. It was as if my subconscious self took over and controlled my mental and physical states. I remember the drive down to MUSC. I live about four hours away, in Greenville, so it was a long, weird drive. I still don’t know how my husband managed to stay so strong and level-headed, all while driving. All I remember is dry-heaving in the car, trying to lay down to relax, and then suddenly sitting back up in the chair anxiously to dry-heave and sob at the same time. My husband tells me he even had to pull off the road one time because we thought I was going to vomit everywhere. I think most of that emotional response was due to the reality I was walking into. My body was so worked up that this was how I responded, whether or not I realized it at the time.
We also sat in one room in the hospital for about six hours after arriving. When I think about that, at the time, it only seemed like two hours. I remember being wheeled downstairs to meet with the anesthesiologist. She had on bright red lipstick. I remember asking her that if I were to die in surgery, I wanted to make sure there was a nurse or someone who could come alongside my husband and help him with details amidst all the chaos. I couldn’t believe I was seriously having that conversation.
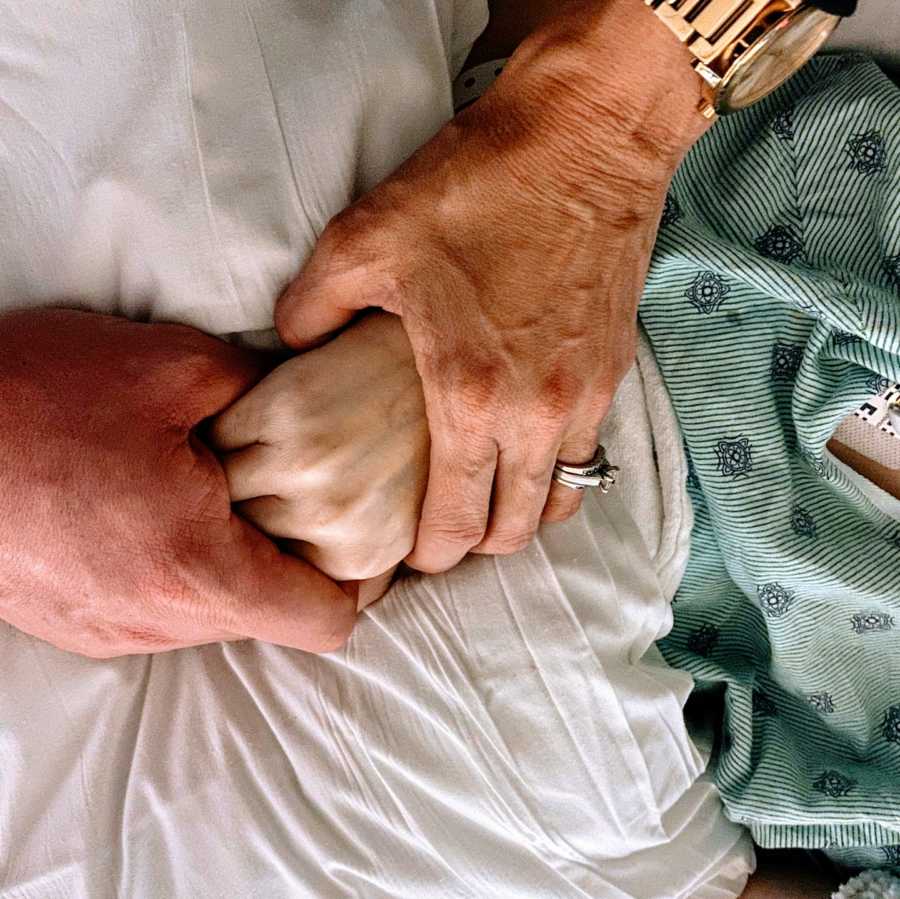
You see, I wasn’t a typical transplant patient. Any transplant is incredibly risky, and death will always be one of those risks. But my blood conditions, as opposite as they are, really threw a lot of uncertainty into my surgery and outcome. There were many questions with doctors and surgeons that went unanswered. No one really knew how these blood conditions would react during an invasive organ transplant. There were so many questions up in the air. But I knew I was the Lord’s, and He held me in His hands. That no matter what happened, if I come away healed with a new liver, or if I die and see Jesus face-to-face, I was okay with either outcome. I was ready. What choice did I have? It’s amazing the strength you can find when you don’t have a choice.
My liver transplant surgery began around 12:00 a.m. on Thanksgiving Day. Pretty ironic timing. My blessing and healing came at the cost of someone else’s tragedy and loss. Here I was, the most thankful I had ever been, yet there was a family who felt the most unthankful at the same time. Sitting down to write my letter to my donor’s family was unlike anything I’ve ever experienced. There is a range of emotions you have and it really is the oddest thing to wrap your head around. I’m over a year post-transplant now, and I have been doing so great. No liver rejection, no complication or issues.


Although I am incredibly thankful and alive because of my liver transplant, it is not an end-all to all of my conditions. It cured my Budd-Chiari liver disease, but I still have to manage my PNH and Polycythemia Vera. I also have to take more medications for life, and those have side effects that come with them. There is no going back to ‘normal’ or to ‘the way things were.’ You have to create a ‘new normal’ after an organ transplant or any chronic medical condition. That change can be difficult mentally and very isolating.
The interesting thing I learned when recovering from my transplant is medical conditions are way more than just physical ailments. I felt like after I received my transplant, my mental state could finally catch up to my physical state. When you’re dealing with medical issues in your body, your physical self is the priority. But really, your mental and emotional self is also just as important, but it doesn’t always get the same attention or time dedicated to it. When I learned of my conditions, I immediately started researching and educating myself on the diseases and parts of my body. But I didn’t have any real idea of the frustrations and limiting abilities to come. The physical aspect of any disease is only one portion of all the stress and chaos that comes with a life transformed by medical necessity. Frustration with appointments and schedules, billing errors and financial stress all occur while still managing the rest of my normal responsibilities as a wife and full-time employee. And don’t even get me started on the topic of a social life. Everyone just thinks your physical state is the only thing affected when you have chronic conditions. But that’s just one third of the stress that a patient endures; the other two thirds are mental and emotional.

But the thing that keeps me going every day and gives me hope is 1) God knows my situation and is in total control because I’ve submitted to Him, and 2) I am not alone. There are others who relate to me. Chronic conditions are very isolating, yes. You feel like no one understands sometimes, and there’s no way for them to truly relate. But there are others out there who, even if they don’t have the same disease, can certainly relate to their life being changed because of a medical condition. Find an online support group and meet people. It’s also important that you advocate for yourself. Partner with your medical team. Do whatever it takes to feel confident in managing your own care. I could talk all day with someone about my experiences and my advice, but we all must sit in our own driver’s seat. Only you can learn what you don’t know; only you can be in charge of how you respond to what is happening to you. Sometimes the isolation that comes with medical conditions are actually blessings in disguise because they push us further than we would have ever gone on our own. Remember, there is always hope. And your story may just be what gives someone else hope.
About the time when I was diagnosed, my husband and I wanted to start our family. I quickly learned my desire to be a mother would have to be put on hold indefinitely. Instead of starting my family like every other normal, young woman, I was told shocking and vital health news. The emotions that came then and still come now, almost four years later, have become a strength I never knew I could experience or yield. Tough situations always provide the opportunity for us to learn something new or to strengthen something already within us. I am a much stronger person in every way today because of what I’ve walked through over the last four years. Struggles in life might be unwanted and hard to overcome, but they always produce gold in us. The struggle produces the will to fight and keep going. It brings about a newfound strength and teaches us how to persevere. Beauty really does come from the ashes.

I learned a lot about myself in walking through these experiences. I have gone through things alone. I have put on a brave face when needed. I have cried by myself on the bathroom floor. But one of the biggest values I have learned is I was always way stronger than I ever thought I could be. So are you. No matter what you face—medical or not—you are so much stronger physically, mentally and emotionally than you ever know. I surprised myself, and I know you will surprise yourself, too.
No one wants to walk through struggles, but it is in those struggles where we learn what we are really made of. That we can keep moving forward. Sometimes you just have to take it day by day, or even hour by hour. But know this: You. Can. Overcome.”

This story was submitted to Love What Matters by Brittany Baughman of Greenville, SC. You can follow her journey on Instagram and her podcast. Submit your own story here, and be sure to subscribe to our free email newsletter for our best stories, and YouTube for our best videos.
Read more stories like this here:
Thank You To My Husband Who Chose To Stay
Provide hope for someone struggling. SHARE this story on Facebook and Instagram to let them know a community of support is available.



